Model No: 124433-A12
Description: Lorem Ipsum is not simply random text.
- SUPERIOR QUALITY
- AFFORDABLE PRICING
- TIMELY SHIPMENT
- CUSTOMER SATISFACTION
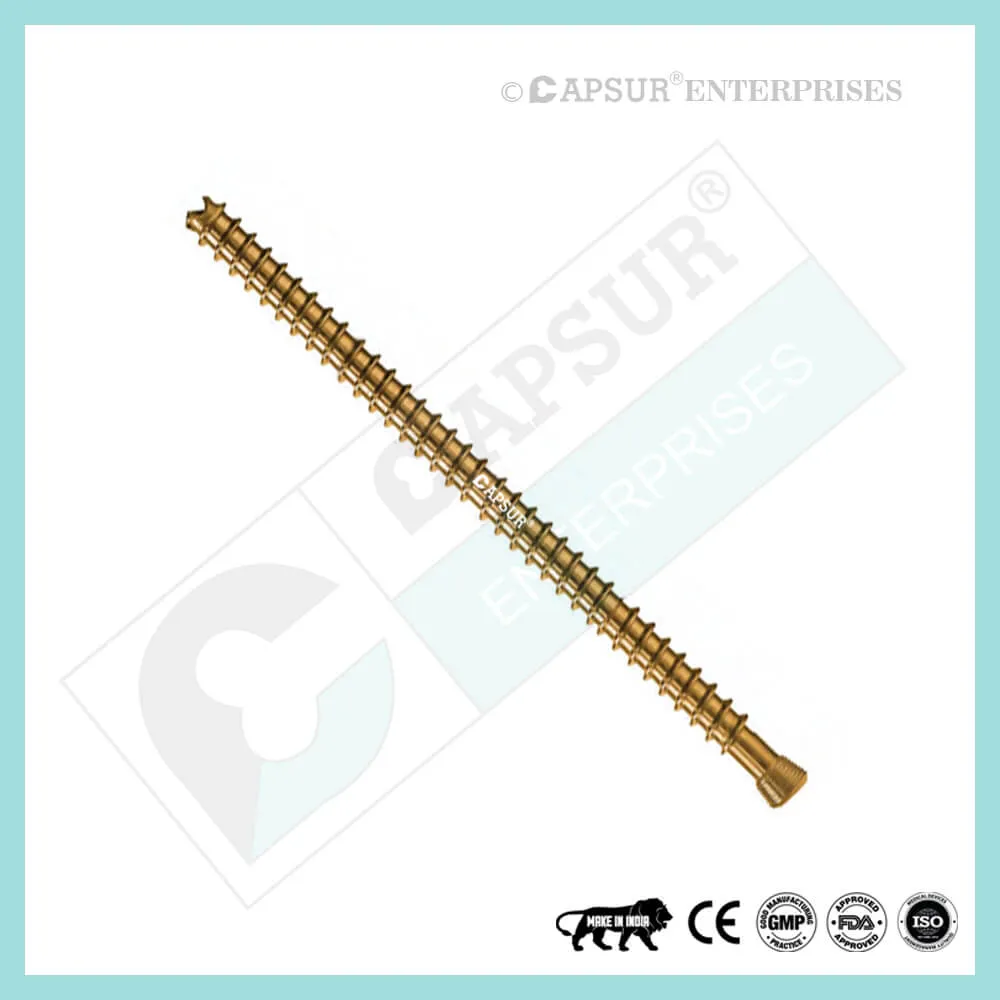
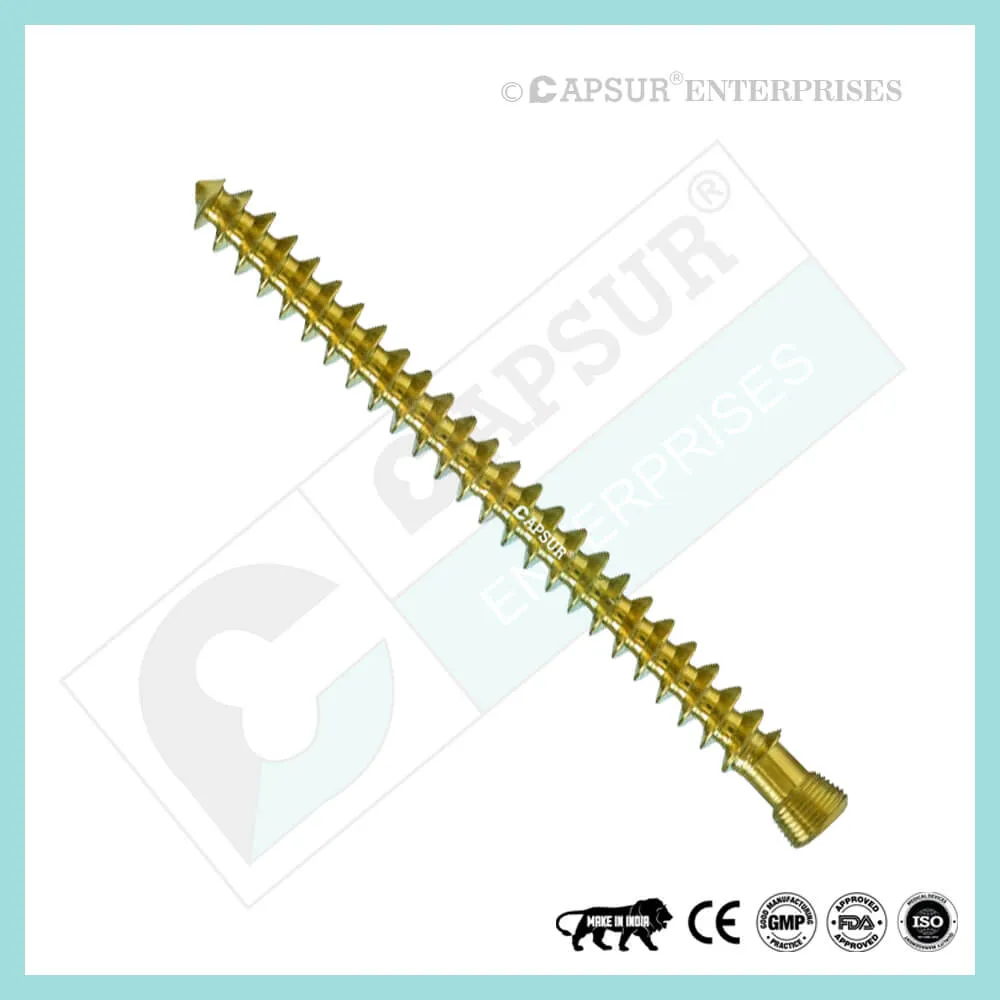
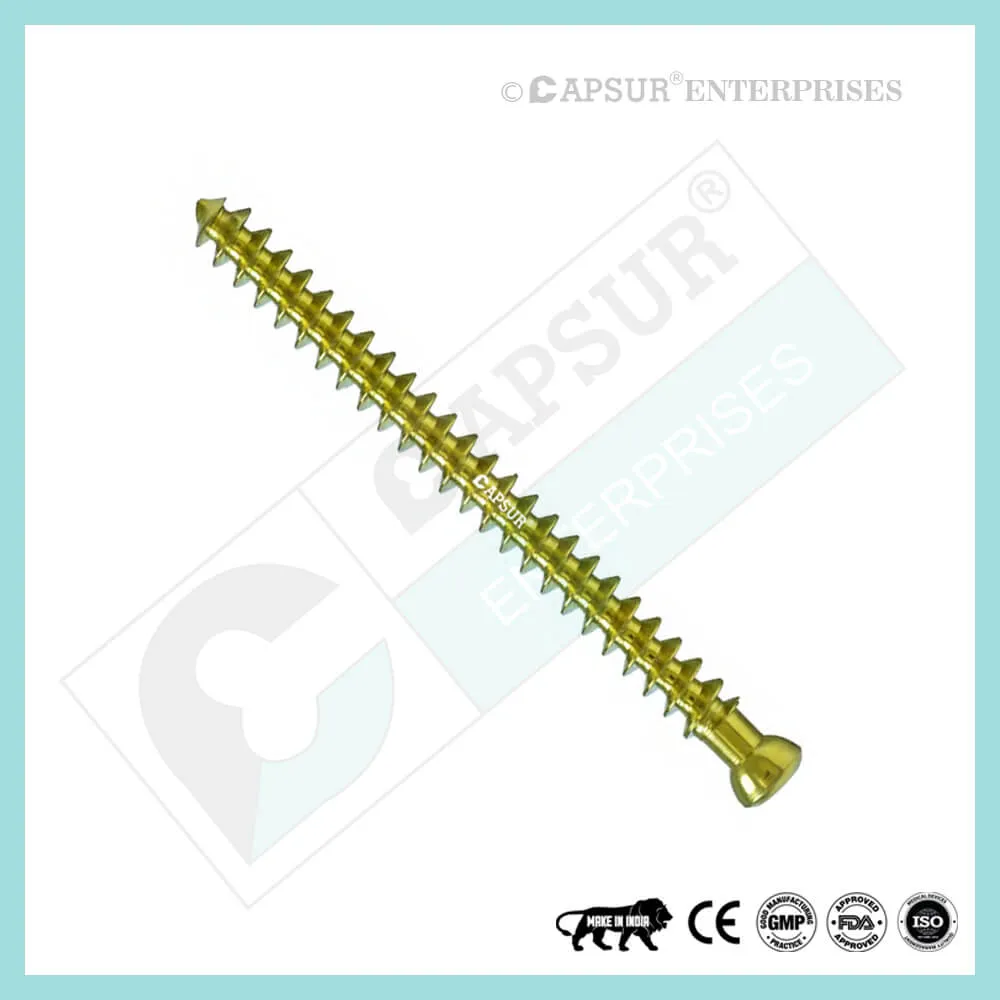
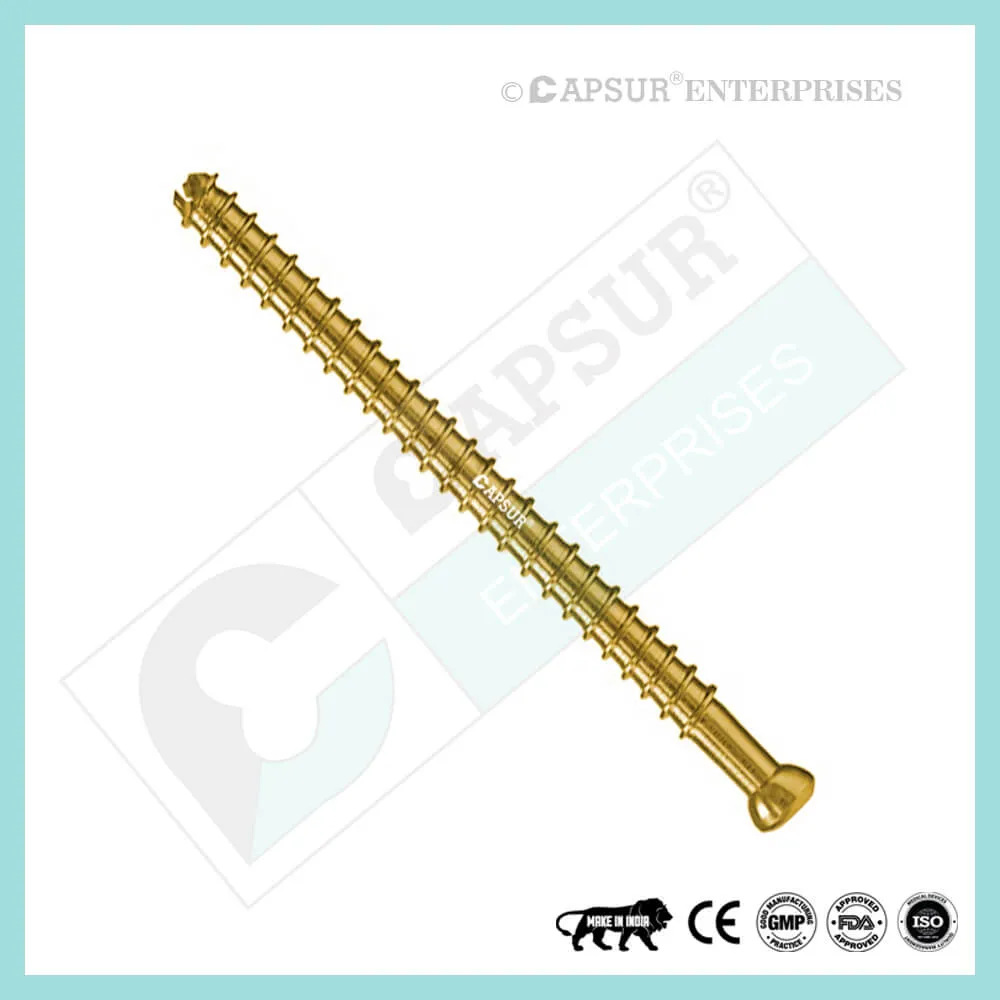
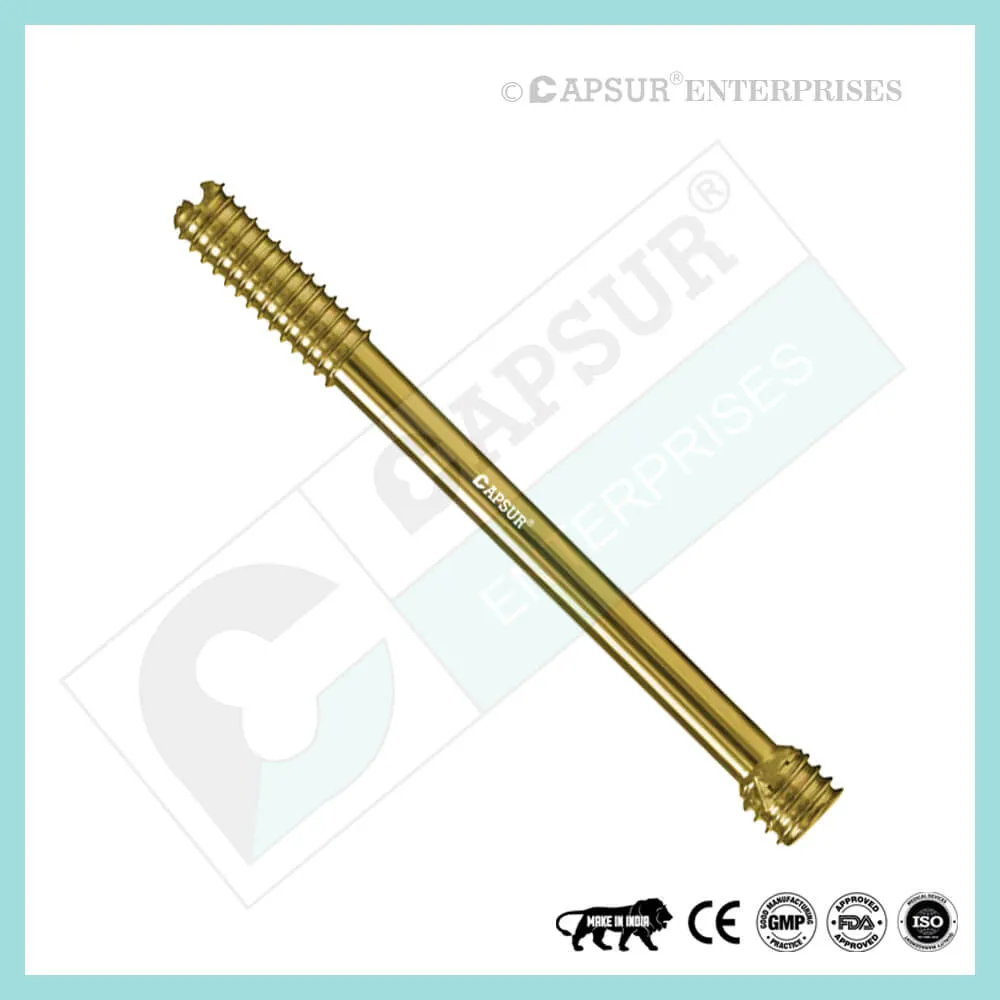
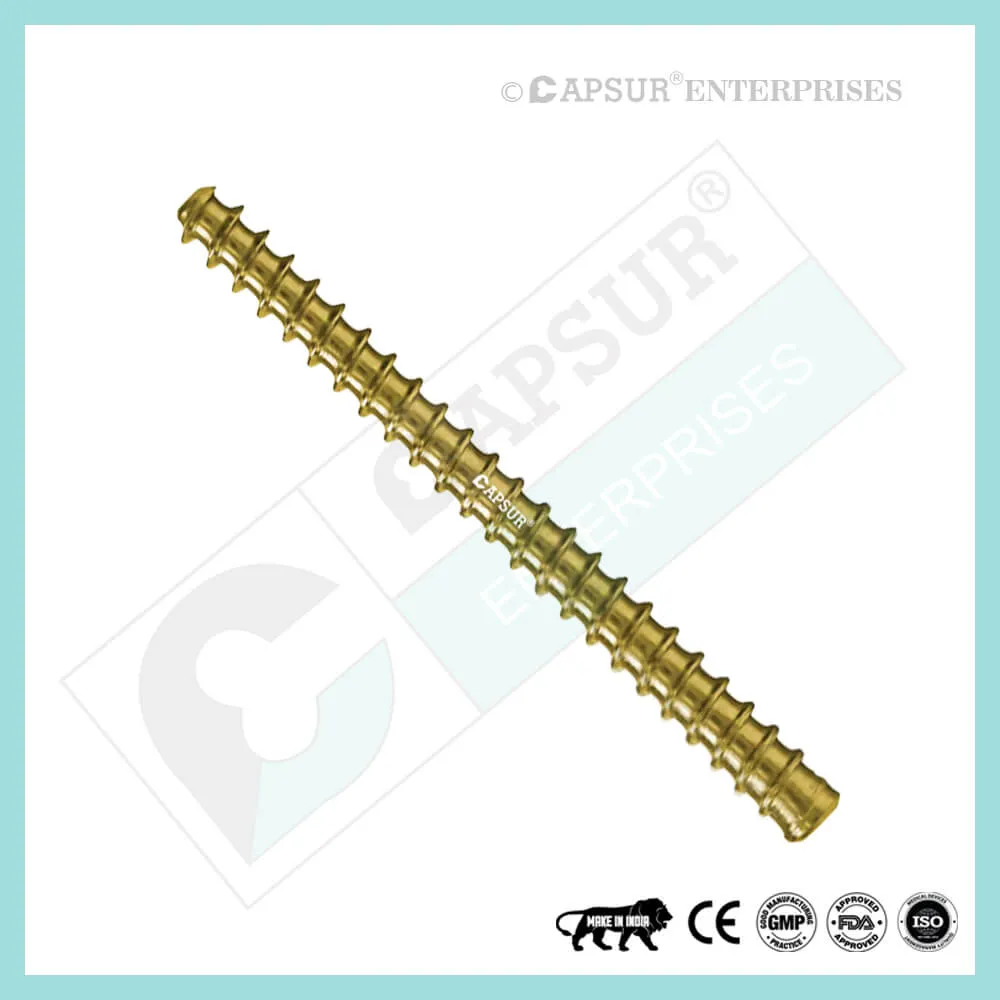
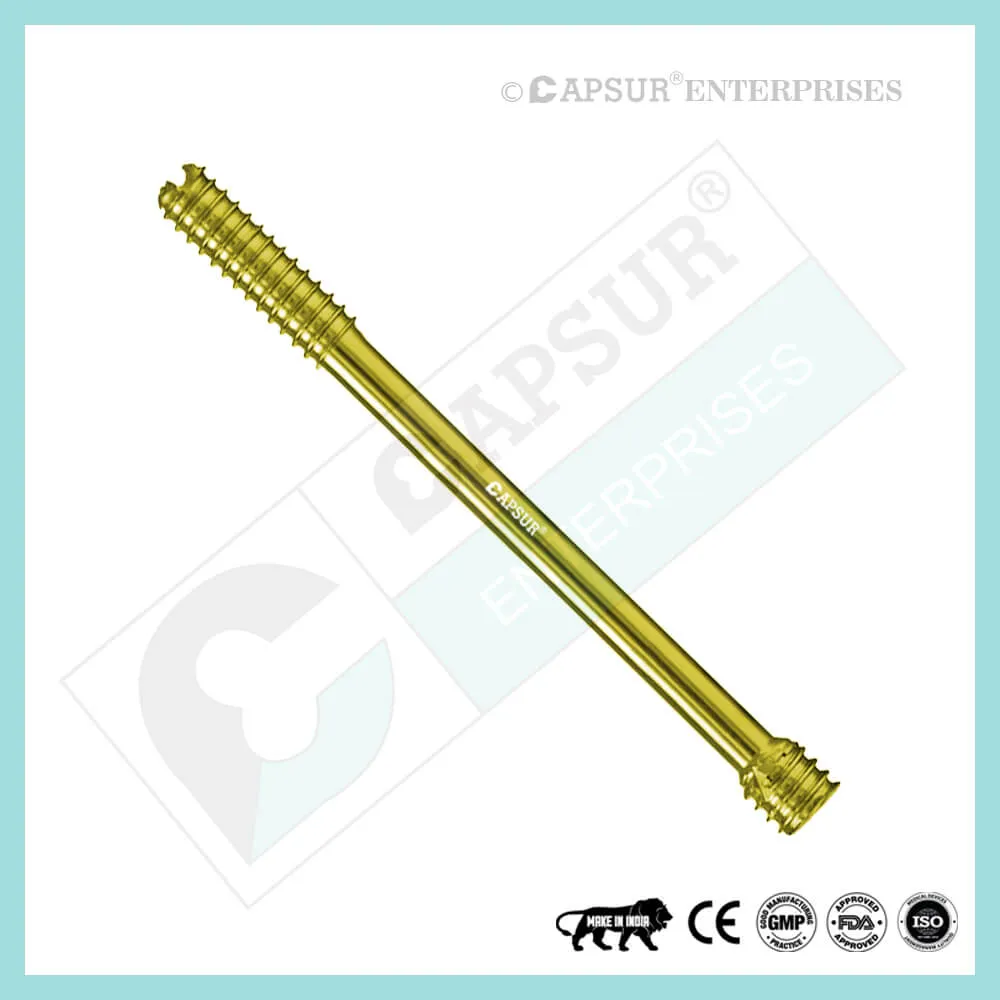
Specification for 2.5 mm Headless Compression Screws, Partially Thread
- The 2.5 mm Headless Compression has a headless design. Screw enables screw implantation in and near articular regions with little risk of causing interference or soft tissue sensitivity.
- inserted precisely using a cannula: Accurate percutaneous insertion with little soft tissue damage is made possible by cannulated designs.
- Variable thread pitch allows for gradual compression: As the screw is advanced, the two fragments are gradually compressed because the screw’s wider thread pitch at the tip penetrates the bone more quickly than its finer trailing threads.
- Fully threaded: A fully threaded screw offers a stronger holding force, enhancing stability.
- Sharp cutting flutes: The screw tip has sharp cutting flutes that make screw insertion easier.
- Screws come in two varieties: fully and partially threaded.
- Available in stainless steel and titanium, the 2.5 mm headless compression screw.
- 8mm, 9mm, 10mm, 11mm, 12mm, 13mm, 14mm, 16mm, 18mm, 20mm, 22mm, 24mm, 26mm, 28mm, and 30mm are the sizes of 2.5 mm Headless Compression Screws that are readily available.
- This screw can be made in any length upon request.
- For this screw, tools like bone taps, combined drill and tap sleeves, counter sinks, depth gauges, drill guides, drill sleeves, hollow mill screw removal tools, reverse measuring devices, screw drivers, and screw holding forceps are all available.
- Self-tapping screw, that is. Self-Tapping Screws create their own thread as they are inserted into the bone. When it enters the bone, it makes a tiny hole that results in a close friction fit between the threads. This prevents vibration-induced loosening and enables the parts’ disassembly if necessary.
- There are sterile and non-sterile packaging choices for headless compression screws.
Uses of 2.5 mm Headless Compression Screws, Partially Thread
- Compression without Heads In accordance with their size, screws can be used for fracture repair, osteotomy, arthrodesis, joint fusion, bone reconstruction, and fracture fixation.
- Headless Compression 2.5 mm Flowing trauma or osteotomies to the hand and foot are intended to be fixed with screws. Screw ends with self-tapping and reverse-cutting flutes make insertion and removal easier. Along its entire length, the tapered profile gains compression and increases pull-out strength.
- Headless Compression 2.5 mm Small bones, bone fragments, and osteotomies are all intended uses for screws as fixation devices. They are not intended for soft tissue fixation or interference.
Other Useful Info of 2.5 mm Headless Compression Screws, Partially Thread
Volar Scaphoid Technique for 2.5 mm Headless Compression Screw
compressed without a head According to their size, screws can be used for joint fusion, bone reconstruction, osteotomies, fracture repair, and fracture fixation of bones.
Compression of 2.5 mm without a head An osteotomy or hand and foot flowing trauma is intended to be fixed with a screw. The screw’s self-tapping and reverse-cutting flutes are designed to make insertion and removal easier. Gaining compression and increasing pull-out strength throughout its length, the tapered profile.
Compression of 2.5 mm without a head Small bones, bone fragments, and osteotomies are intended to be fixed with screws. They are not meant to cause interference or fix soft tissue.
Dorsal Scaphoid Technique for 2.5 mm Headless Compression Screw
- ATTITUDE AND NEEDLE INSTALLATION
At the tip of the scaphoid, close to the scapholunate ligament, is where the entry point into the proximal pole is located. This can be located between the third and fourth extensor compartments using an arthroscopy or a mini open dorsal approach. Whatever method is used, it is crucial to watch out for the guide wire transfixing an extensor tendon.
Once the entry point has been determined, insert the proper guide wire, aiming for the base of the thumb, and check the position on the fluoroscope. The subchondral surface of the distal pole of the scaphoid should be where the leading edge of the guide wire is positioned. Verify the depth and placement of the wire during imaging.
2. FRACTION STABILIZATION
The placement of a second parallel guide wire using the parallel wire guides may be beneficial if the fracture is unstable.
- FIGURE OUT SCREW LENGTH
The percutaneous screw sizer or the placement of a second wire at the entry point and the subtraction of the difference are both methods for measuring guide wire length. Due to the restricted access, the screw sizer cannot be used with the arthroscopic technique. To make sure that both screw ends are buried in the bone, deduct 4 mm from the measured length.
- DIRECT WIRE IN ADVANCE
The guide wire should be advanced through the distant cortex until it is in the subcutaneous tissues. This reduces the possibility of the guide wire accidentally being withdrawn during drilling and makes it easier to remove the wire if it breaks.
Tip: The screw shouldn’t be longer than 26 mm for the majority of adult males and 22 mm for females.
- DRILL CORTEX-FREE
With the right profile drill, the near cortex can be opened.
- FAR FRAGMENT DRILL
Next, use the long drill to enlarge the far fragment. The drill only needs to move 4-5 mm past the fracture site in order to be effective.
Advice: To lessen the effects of varying bone density and distraction during screw insertion, use a long drill.
7. SCREW INSERTION
Use the proper hex driver and the correct-sized screw to insert. Stop, remove the screw, redrill with the long drill, and then re-insert the screw if resistance is encountered during insertion or if a distraction occurs. Verify the screw’s position and length on imaging, making sure that the leading and trailing edges are buried beneath the articular surfaces. At last, take the guide wires out.
Different Types of Screws including 2.5 mm Headless Compression Screw
Locking Cortical Screws
- 2 mm Locking Cortical Screws
- 2.4 mm Locking Cortical Screws
- 2.7 mm Locking Cortical Screws
- 3.5 mm Locking Cortical Screws
- 5 mm Locking Cortical Screws
Cortical Screws
- 1.5 mm Cortical Screws
- 2 mm Cortical Screws
- 2.4 mm Cortical Screws
- 2.7 mm Cortical Screws
- 3.5 mm Cortical Screws
- 4.5 mm Cortical Screws
Locking Cancellous Screws
- 3.5 mm Locking Cancellous Screw
- 4 mm Locking Cancellous Screw
- 5 mm Locking Cancellous Screw
- 6.5 mm Locking Cancellous Screw
Cancellous Screws
- 3.5 mm Cancellous Screw
- 4 mm Cancellous Screw
- 6.5 mm Cancellous Screw
- Locking Cannulated Screws
- 4 mm Locking Cannulated Screw
- 5 mm Locking Cannulated Screw
- 6.5 mm Locking Cannulated Cancellous Screw
- 7.3 mm Locking Cannulated Cancellous Screw
Cannulated Screws
- 3.5 mm Cannulated Screws (Cortical Thread)
- 4 mm Cannulated Cancellous Screws
- 4.5 mm Cannulated Cancellous Screws
- 6.5 mm Cannulated Cancellous Screws
- 7 mm Cannulated Cancellous Screws
- 7.3 mm Cannulated Cancellous Screws
Headless Screws Full Thread
- 2.5 mm Headless Compression Screws Full Thread
- 3 mm Headless Compression Screws Full Thread
- 3.5 mm Headless Compression Screws Full Thread
- 4 mm Headless Compression Screws Full Thread
- 4.5 mm Headless Compression Screws Full Thread
- 5 mm Headless Compression Screws Full Thread
- 5.5 mm Headless Compression Screws Full Thread
- 6.5 mm Headless Compression Screws Full Thread
Headless Screws Partially Thread
- 2.5 mm Headless Compression Screws Partially Thread
- 3 mm Headless Compression Screws Partially Thread
- 3.5 mm Headless Compression Screws Partially Thread
- 4 mm Headless Compression Screws Partially Thread
- 4.5 mm Headless Compression Screws Partially Thread
- 5.5 mm Headless Compression Screws Partially Thread
- 6.5 mm Headless Compression Screws Partially Thread
- 7.5 mm Headless Compression Screw Partially Thread
Interlocking Nail Screws
PFNA2 Blades
PFNA Blades
- 8 mm Proximal Cannulated Bolt
- 6.4 mm Proximal Cannulated Bolt
- 4.9 mm Locking Bolts
- 3.9 mm Locking Bolts
- 3.4 mm Locking Bolts
Interference Screws
- 5 mm Interference Screw
- 6 mm Interference Screw
- 7 mm Interference Screw
- 8 mm Interference Screw
- 9 mm Interference Screw
- 10 mm Interference Screw
Herbert Screws
- 2.5 mm Cannulated Herbert Screws
- 3 mm Cannulated Herbert Screws
- 3.5 mm Cannulated Herbert Screws
- 4.5 mm Cannulated Herbert Screws
- 5.5 mm Cannulated Herbert Screws
- 6.5 mm Cannulated Herbert Screws
Craniomaxillofacial Screws
- 1.5 mm Screw Craniomaxillofacial
- 2 mm Screw Craniomaxillofacial
- 2 mm Locking Screw Craniomaxillofacial
- 2.5 mm Screw Craniomaxillofacial
- 2.5 mm Locking Screw Craniomaxillofacial
- 2.8 mm Screw Craniomaxillofacial
- 2.8 mm Locking Screw Craniomaxillofacial
- 2.7 mm Emergency Screw
Malleolar Screws
- 3.5 mm Malleolar Screws
- 4.5 mm Malleolar Screws
The most frequently used orthopedic implants are bone screws. For various types of bones, there are numerous types and sizes of screws. The majority of bone screws are constructed from titanium or stainless steel alloys. When determining screw mechanics, it’s important to consider the outer diameter, root diameter, thread pitch, and angle.
A screw’s outer diameter is commonly used in orthopedics to describe it. For instance, a “2.5 mm Headless Compression Screw” has an outer diameter of 2.5 mm. The linear distance covered by a screw during one complete turn is known as the pitch of the screw. With each full turn, the screw moves forward by a distance equal to the space between the threads. Cortical screws have more threads because they have a lower pitch. Given the fragility of the bone, cancellous bone screws have a deeper screw to increase surface area and enhance purchase.
Screws work by converting the torque applied to tighten them into internal tension and elastic responses in the bone around them. The fracture fragments that the screw is holding together are compressed as a result. Typically, screws are inserted into holes that have been drilled to the same diameter as the root and are either self-tapping or have been tapped (threaded) beforehand. The screws must be properly inserted into the proper size drilled hole and made to withstand the insertion torque levels anticipated in cortical bone because the torque to insert cortical bone screws can be high. Large, deep threads on cancellous bone screws allow them to securely hold the spongy bone. It is uncommon for a screw to fail during insertion due to the cancellous bone’s relatively low strength, but pull out can be problematic.
2.5 mm Headless Compression Screw Risk Factor
When assessing the prognosis in each case, contraindications—which may be partial or complete—must be taken into account. Under the following circumstances, alternative management strategies may need to be taken into account:
- infections that are systemic or local, acute or chronic.
- either localized, systemic, or chronic inflammation.
- serve as a dangerous vascular, nervous, or muscular disease.
- Bone defects that would prevent the implant from being properly anchored.
- All associated illnesses that might jeopardize the implant’s success and functionality.
Warnings and Precautionary for 2.5 mm Headless Compression Screw
The surgeon and support staff should read the safety instructions in this document as well as any product-specific information in the product description, surgical techniques, and/or brochures before using 2.5 mm Headless Compression Screw.
Screws are designed, built, and produced with the utmost care using materials of the highest quality for medical use. If these high-quality screws are used properly, they guarantee the best working outcomes. As a result, the usage guidelines and safety advice below must be followed.
The incorrect use of a screw can result in injury to the operator, patients, or other people as well as tissue damage, premature wear and tear, instrument destruction, and instrument destruction.
The operating surgeon must actively participate in the medical care of their patients. The surgeon must have a complete understanding of the instruments, their limitations, and the surgical procedure. The surgeon and the surgical team are responsible for exercising caution in the selection and use of surgical instruments. Before using implants, adequate surgical training should be obtained.
Factors that could harm the operation’s success include:
- allergies to materials implanted.
- regional bone tumors.
- osteomalacia or osteoporosis.
- metabolic disturbances and systemic disease.
- drug and alcohol abuse.
- Excessive shock-producing physical activity that exposes the implant to blows and/or heavy loads.
- Patients who lack the mental capacity to comprehend and follow instructions from a doctor.
- Unhealthy overall.
- Potential Negative Effects
The most frequent side effects following implantation are as follows:
- screw loosening that may be caused by the implant’s tissue reaction or by the fixation site’s repeated loading.
- the two stages of infection.
- additional bone fracture brought on by abnormal stress or weakened bone structure.
- a hematoma or pressure-related pressure that causes temporary or permanent neural damage.
- Hematomas from wounds and slow wound healing.
- Venous thrombosis, pulmonary embolism, and cardiac arrest are examples of vascular disease.
- heterotopically ossifying.
- Due to the presence of the 2.5 mm Headless Compression Screw, there is pain and discomfort.
- Implant mechanical failure, such as bending, loosening, or breakage.
- Implant migration leading to injury.
Preoperative Planning for 2.5 mm Headless Compression Screw
A thorough clinical evaluation of the patient is followed by the execution of the operating plan. X-rays are also required to provide a clear picture of the bony anatomy and any associated deformities. The appropriate implantation tools and a full size 2.5 mm Headless Compression Screw must be on hand at the time of the procedure.
The patient should be informed of any potential risks and side effects related to implant use by the clinician. It is critical to ascertain the patient’s allergy status to all implant materials prior to surgery. The patient must also be made aware that the device’s performance cannot be guaranteed because problems may shorten the device’s useful life.
2.5 mm Headless Compression Screw Precautions
During reprocessing, verify that the instruments are functional and look for wear. Before using, replace any worn-out or broken instruments.
It is advised to use the tools designated for this screw.
Use caution when handling equipment, and put used bone-cutting tools in a sharps container.
Always use suction and irrigation to remove any debris that may be produced during implantation or removal.
2.5 mm Headless Compression Screw Warnings
Headless Compression 2.5 mm During use, a screw may break (if excessive forces are applied). We advise that the broken part be removed whenever possible and practical for the particular patient, though the surgeon will ultimately decide whether to do so based on the risk involved. Be aware that implants lack the natural bone’s strength. Significant loads may cause implants to fail.
The user’s glove or skin may be pinched or torn by the sharp edges or moving joints of some instruments, screws, and cut plates.
Be sure to get rid of any fragments that weren’t fixed during surgery.
While the surgeon will ultimately decide whether to remove the implant, we advise that fixation devices be taken out as soon as it is safe and practical for the specific patient and after their purpose as a healing aid has been fulfilled. To prevent refracture, implant removal should be followed by adequate post-operative care.
2.5 mm Headless Compression Screw General Adverse Events
There are risks, side effects, and adverse events associated with all major surgical procedures. While there are many possible reactions, the following are some of the most frequent ones: issues related to anesthesia and patient positioning (such as nausea, vomiting, dental injuries, neurological impairments, etc.), thrombosis, embolism, infection, damage to nerve and/or tooth roots or other critical structures, such as blood vessels, excessive bleeding, damage to soft tissues, including swelling, abnormal scar formation, functional impairment of the musculoskeletal system, and pain.
| 2.5 mm Headless Compression Screws, Partially Thread |
|---|