Model No: 124433-A12
Description:
- SUPERIOR QUALITY
- AFFORDABLE PRICING
- TIMELY SHIPMENT
- CUSTOMER SATISFACTION
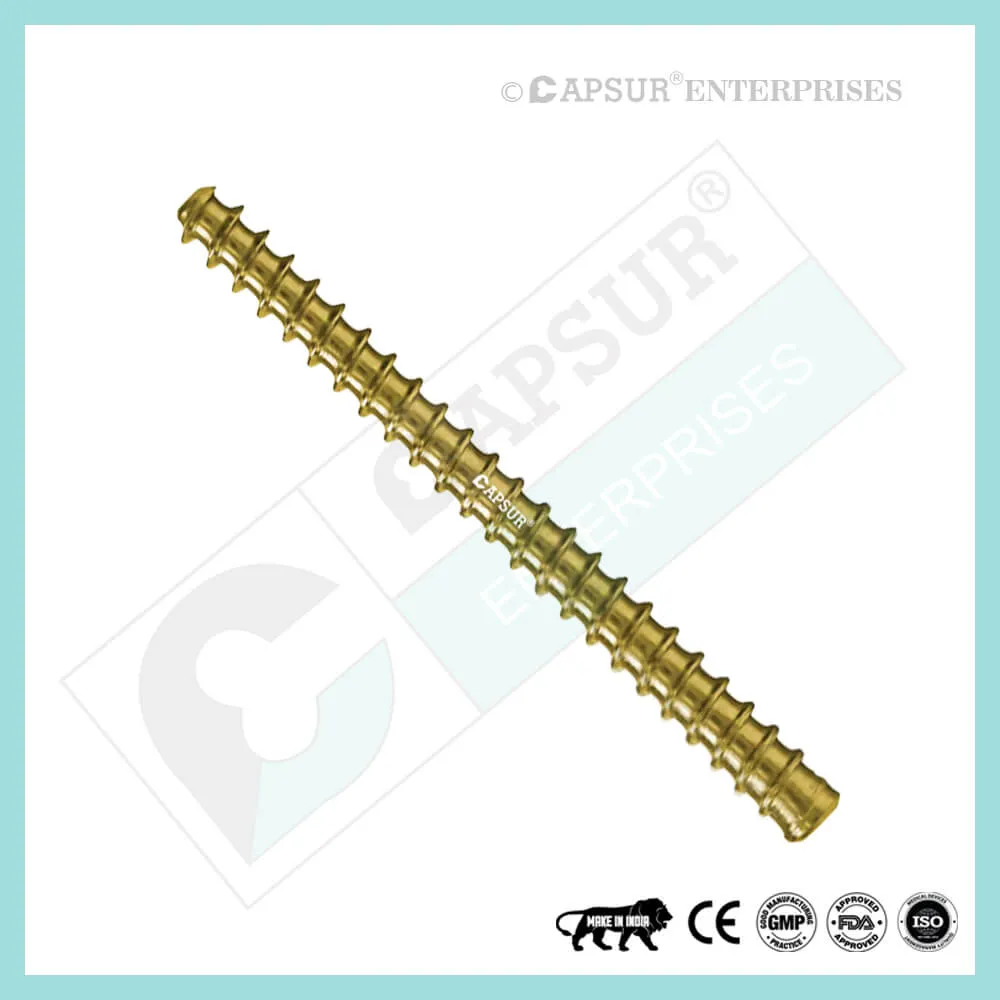
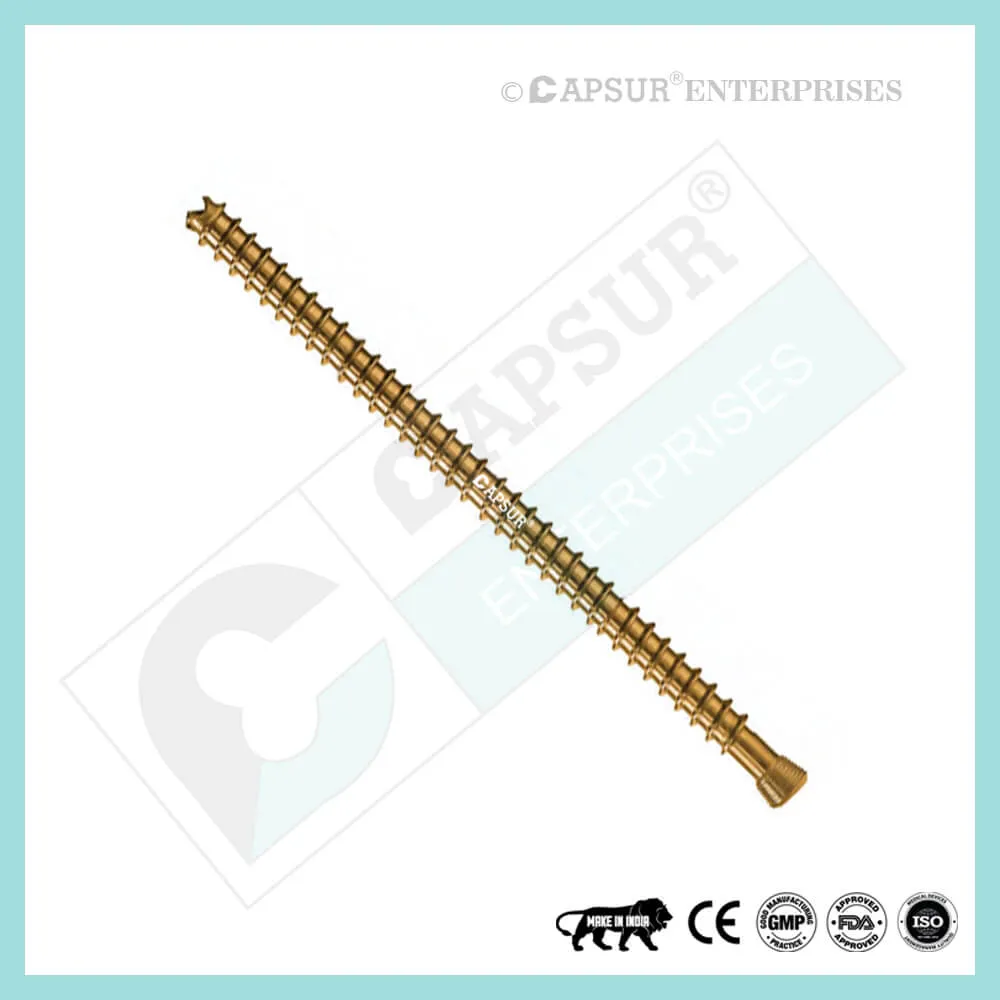
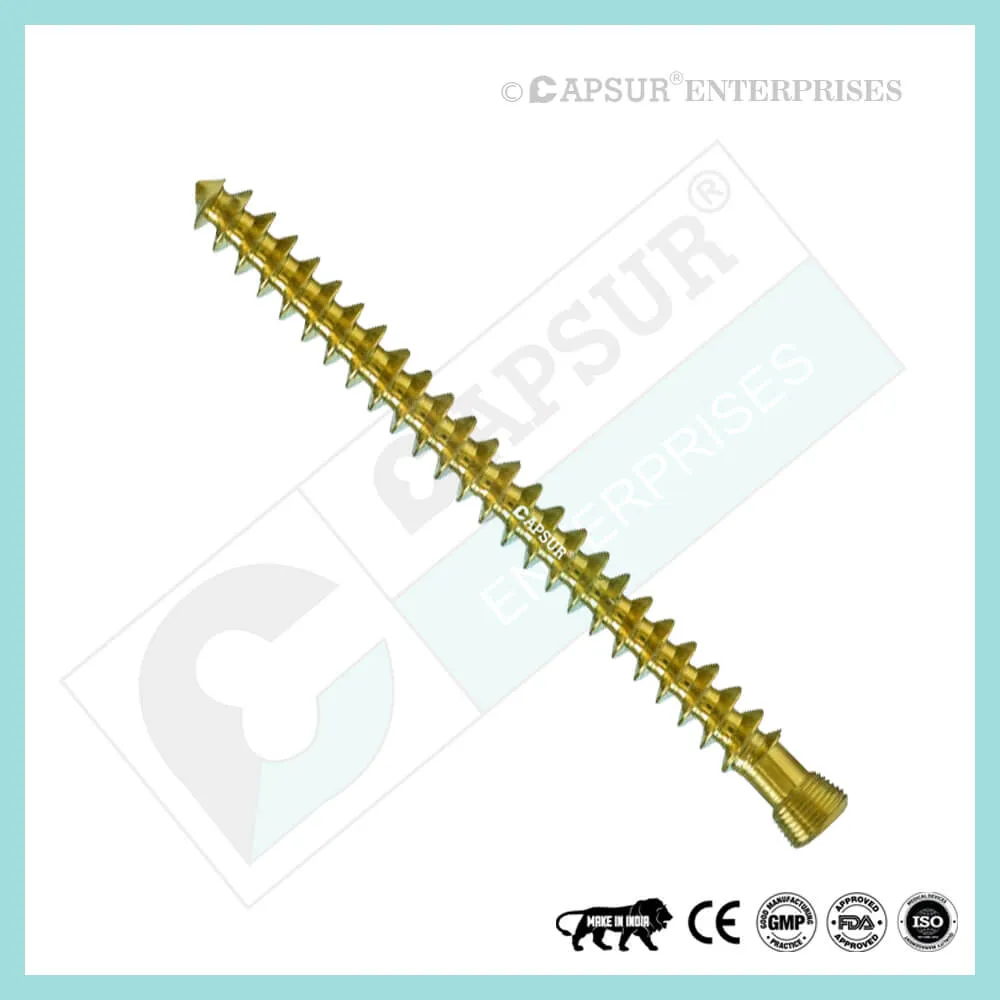
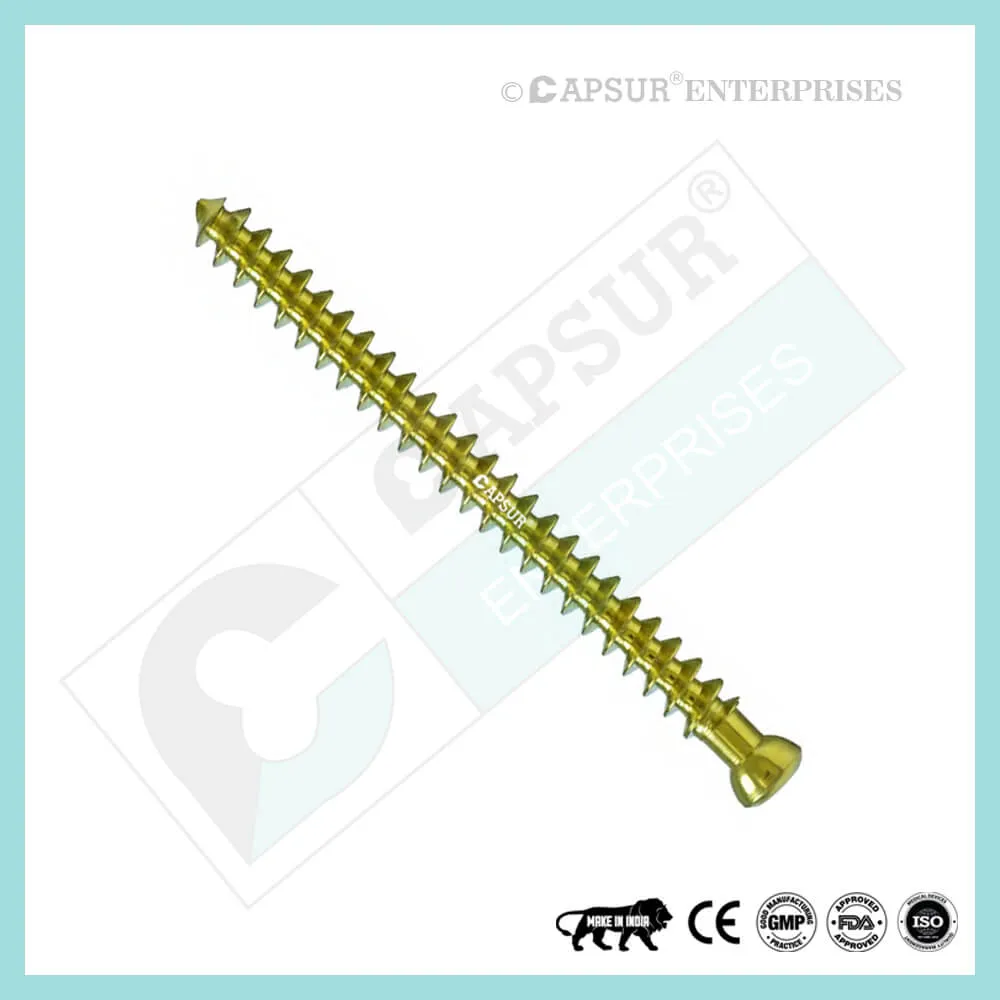
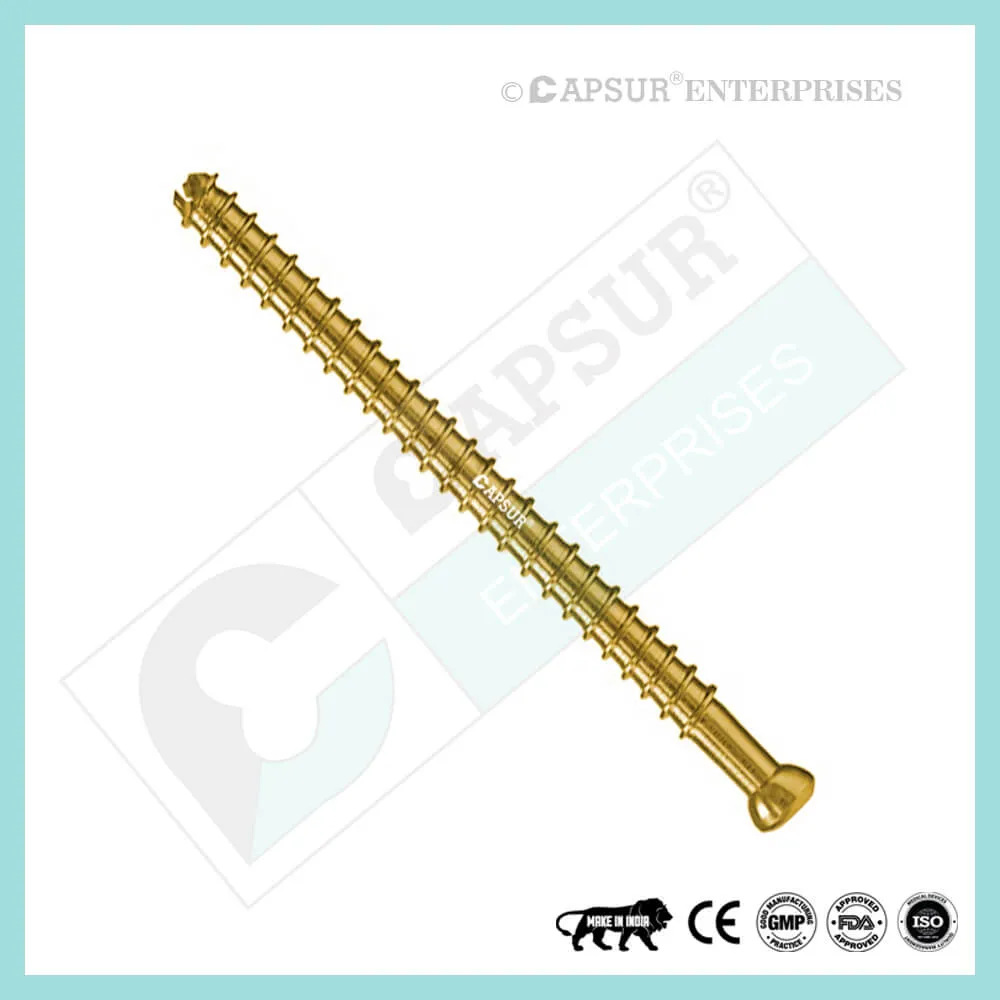
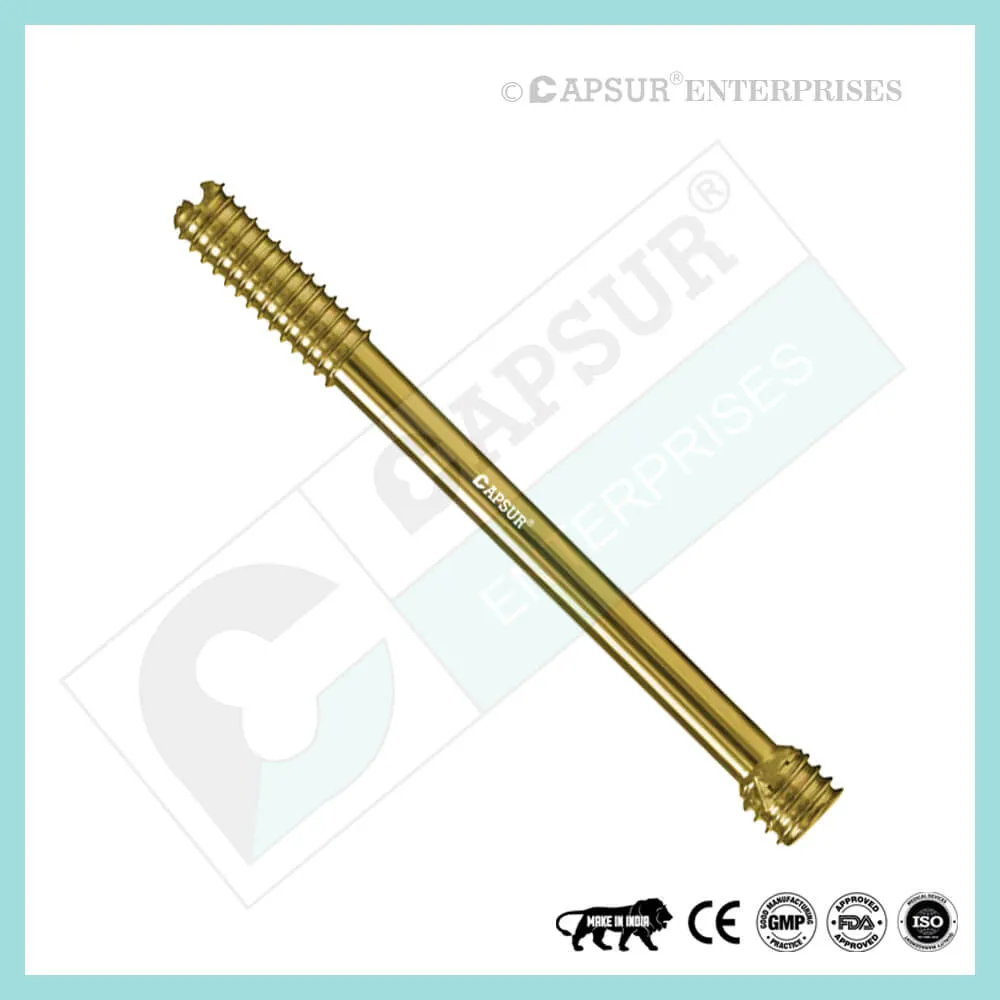
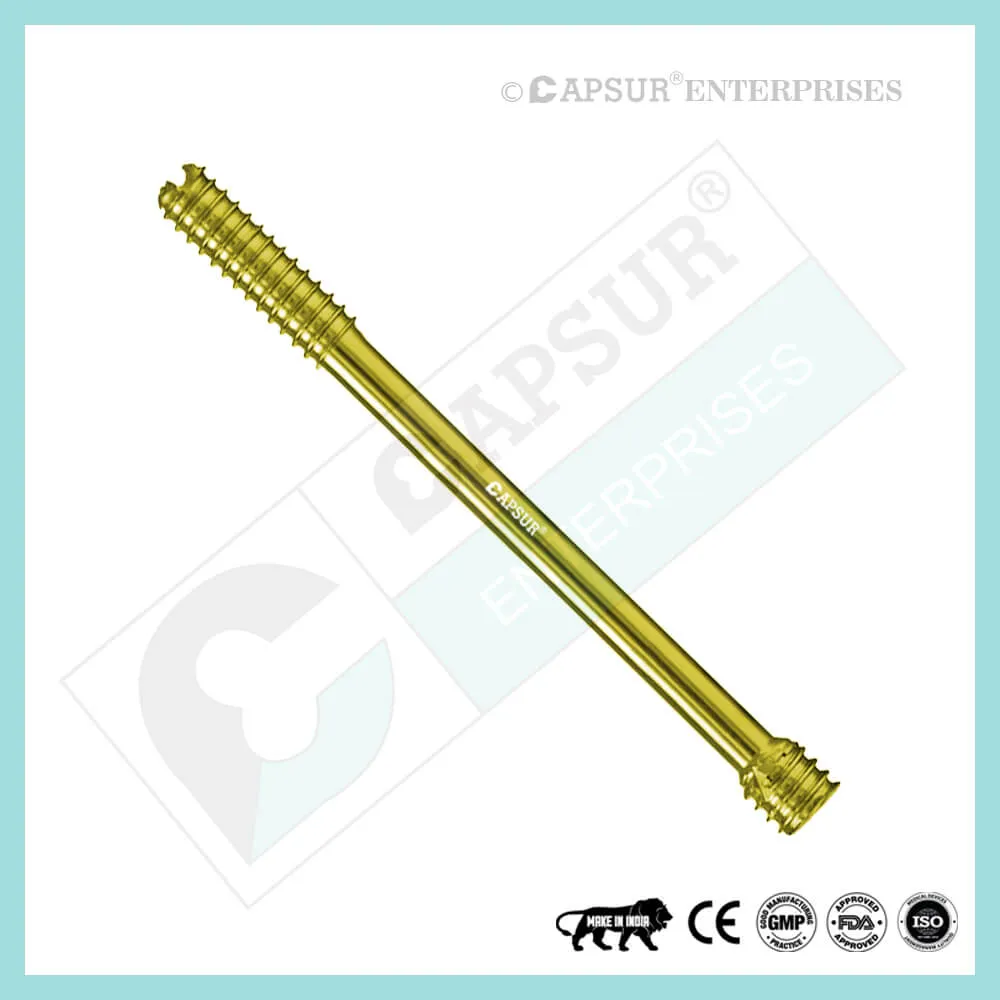
Specification for 7.5 mm Headless Compression Screws, Full Thread
- Design without a head: 6.5 mm headless design compressed without a head Screw enables screw implantation in and near articular regions with little risk of causing interference or soft tissue sensitivity.
- A cannulated design facilitates accurate percutaneous insertion with the least amount of soft tissue damage.
- Variable thread pitch allows for gradual compression: As the screw is advanced, the two fragments are gradually compressed because the screw’s wider thread pitch at the tip penetrates the bone more quickly than its finer trailing threads.
- Fully threaded: A fully threaded screw offers a stronger holding force, enhancing stability.
- Sharp cutting flutes: The screw tip has sharp cutting flutes that make screw insertion easier.
- Screws come in two varieties: fully and partially threaded.
- Available in stainless steel and titanium, the 7.5 mm headless compression screw.
- Compression of 7.5 mm without a head 25mm, 30mm, 35mm, 40mm, 45mm, 50mm, 55mm, 60mm, 65mm, 70mm, 75mm, 80mm, 85mm, 90mm, 95mm, 100mm, 105mm, 110mm, 115mm, and 120mm are the screw sizes that are readily available.
- This screw can be made in any length upon request.
- For this screw, tools like bone taps, combined drill and tap sleeves, counter sinks, depth gauges, drill guides, drill sleeves, hollow mill screw removal tools, reverse measuring devices, screw drivers, and screw holding forceps are all available.
- Self-tapping screw, that is. Self-Tapping Screws create their own thread as they are inserted into the bone. When it enters the bone, it makes a tiny hole that results in a close friction fit between the threads. This prevents vibration-induced loosening and enables the parts’ disassembly if necessary.
- There are sterile and non-sterile packaging choices for headless compression screws.
Uses of 7.5 mm Headless Compression Screws, Full Thread
- Compression without Heads In accordance with their size, screws can be used for fracture repair, osteotomy, arthrodesis, joint fusion, bone reconstruction, and fracture fixation.
- Headless Compression, 7.5 mm Flowing trauma or osteotomies to the hand and foot are intended to be fixed with screws. Screw ends with self-tapping and reverse-cutting flutes make insertion and removal easier. Along its entire length, the tapered profile gains compression and increases pull-out strength.
- Headless Compression, 7.5 mm The clavicle, humerus, radius, ulna, ilium, femur, patella, fibula, tibia, talus, malleolus, and calcaneus are among the bones that can be fused, fractured, or osteotomized using a screw.
Other Useful Info of 7.5 mm Headless Compression Screws, Full Thread
7.5 mm Headless Compression Screws Surgical Techniques
PATIENT POSITIONING, first
Using a bean bag body positioner, place the patient in a semi-lateral position. The operative leg should be draped freely with the up position, and the patient should be moved to the far end of the bed. Before prep and drape, the operative limb should be tested for exertion to ensure that it can be placed on the mini c-arm during surgery.
- OUTLINE OF THE INDICATION AREA
The insertions of the peroneus brevis and tertius tendons, as well as the base of the fifth metatarsal, are indicated.
- ARRANGEMENT AND EXPOSURE
Under fluoroscopic guidance, the.062′′ guide wire for the 4.7 Screw can be placed at the base of the fifth metatarsal. The peroneus brevis and tertius tendons meet at the base of the fifth metatarsal, where a small incision is made. The sural nerve branches that cross the peroneal tendons are carefully noted and guarded. It may be necessary to separate and retract the fibers of the peroneus brevis and lateral aponeurosis tendon away from the styloid process of the base of the fifth metatarsal. On the plantar aspect of the base of the fifth metatarsal, a miniature Hohman retractor is positioned. By inserting their fingers between the fourth and fifth metatarsals, the surgeon can reduce the fifth metatarsal fracture. By doing this, the fifth metatarsal fracture site is sealed off while the guide wire, drill, and screw are being inserted. From the fifth metatarsal’s base into the metatarsal shaft’s middle, a guide wire is drilled. In order to prevent distal penetration, it is kept within the intramedullary canal. Use fluoroscopy to confirm placement.
- ESTIMATE DEPTH
Using a cannulated depth gauge, depth is determined from the guide wire’s exposed end.
- GUIDE WIRE IN ADVANCE
To maintain distal pin fixation before drilling, advance the guide wire by about 5 mm after choosing the size.
When advancing the guide wire, exercise caution to avoid damaging the surfaces of the distal joint.
- PLACEMENT OF SOFT TISSUE GUIDE
Utilizing the appropriate cannulated profile drill, position the soft tissue guide (which should be used throughout) over the guide wire and open the near cortex.
- DRILL
Drill the appropriate cannulated, long drill into the far fragment while leaving the soft tissue guide in place. To confirm the desired depth, check the markings on the drill.
Advice: To lessen the effects of varying bone density and distraction during screw insertion, use a long drill.
- COMPRESSION OF FRACTIONS
A screw that is 5 mm shorter than the measured total depth is inserted over the guide wire while shielding the soft tissues with a soft tissue guide in order to account for countersinking and fracture compression.
- INSERTING A SCREW
To prevent cortical penetration, the screw is placed under fluoroscopic guidance. postoperative guidelines: A fiberglass splint is used to support the patient as they are covered in a soft dressing. Depending on the type of fracture, the quality of the bone, and any underlying morbidities, patients may be made non-weight-bearing for a period of 2 to 6 weeks after surgery.
Different Types of Screws including 7.5 mm Headless Compression Screw
Locking Cortical Screws
- 2 mm Locking Cortical Screws
- 2.4 mm Locking Cortical Screws
- 2.7 mm Locking Cortical Screws
- 3.5 mm Locking Cortical Screws
- 5 mm Locking Cortical Screws
Cortical Screws
- 1.5 mm Cortical Screws
- 2 mm Cortical Screws
- 2.4 mm Cortical Screws
- 2.7 mm Cortical Screws
- 3.5 mm Cortical Screws
- 4.5 mm Cortical Screws
Locking Cancellous Screws
- 3.5 mm Locking Cancellous Screw
- 4 mm Locking Cancellous Screw
- 5 mm Locking Cancellous Screw
- 6.5 mm Locking Cancellous Screw
Cancellous Screws
- 3.5 mm Cancellous Screw
- 4 mm Cancellous Screw
- 6.5 mm Cancellous Screw
- Locking Cannulated Screws
- 4 mm Locking Cannulated Screw
- 5 mm Locking Cannulated Screw
- 6.5 mm Locking Cannulated Cancellous Screw
- 7.3 mm Locking Cannulated Cancellous Screw
Cannulated Screws
- 3.5 mm Cannulated Screws (Cortical Thread)
- 4 mm Cannulated Cancellous Screws
- 4.5 mm Cannulated Cancellous Screws
- 6.5 mm Cannulated Cancellous Screws
- 7 mm Cannulated Cancellous Screws
- 7.3 mm Cannulated Cancellous Screws
Headless Screws Full Thread
- 2.5 mm Headless Compression Screws Full Thread
- 3 mm Headless Compression Screws Full Thread
- 3.5 mm Headless Compression Screws Full Thread
- 4 mm Headless Compression Screws Full Thread
- 4.5 mm Headless Compression Screws Full Thread
- 5 mm Headless Compression Screws Full Thread
- 5.5 mm Headless Compression Screws Full Thread
- 6.5 mm Headless Compression Screws Full Thread
Headless Screws Partially Thread
- 2.5 mm Headless Compression Screws Partially Thread
- 3 mm Headless Compression Screws Partially Thread
- 3.5 mm Headless Compression Screws Partially Thread
- 4 mm Headless Compression Screws Partially Thread
- 4.5 mm Headless Compression Screws Partially Thread
- 5.5 mm Headless Compression Screws Partially Thread
- 6.5 mm Headless Compression Screws Partially Thread
- 7.5 mm Headless Compression Screw Partially Thread
Interlocking Nail Screws
PFNA2 Blades
PFNA Blades
- 8 mm Proximal Cannulated Bolt
- 6.4 mm Proximal Cannulated Bolt
- 4.9 mm Locking Bolts
- 3.9 mm Locking Bolts
- 3.4 mm Locking Bolts
Interference Screws
- 5 mm Interference Screw
- 6 mm Interference Screw
- 7 mm Interference Screw
- 8 mm Interference Screw
- 9 mm Interference Screw
- 10 mm Interference Screw
Herbert Screws
- 2.5 mm Cannulated Herbert Screws
- 3 mm Cannulated Herbert Screws
- 3.5 mm Cannulated Herbert Screws
- 4.5 mm Cannulated Herbert Screws
- 5.5 mm Cannulated Herbert Screws
- 6.5 mm Cannulated Herbert Screws
Craniomaxillofacial Screws
- 1.5 mm Screw Craniomaxillofacial
- 2 mm Screw Craniomaxillofacial
- 2 mm Locking Screw Craniomaxillofacial
- 2.5 mm Screw Craniomaxillofacial
- 2.5 mm Locking Screw Craniomaxillofacial
- 2.8 mm Screw Craniomaxillofacial
- 2.8 mm Locking Screw Craniomaxillofacial
- 2.7 mm Emergency Screw
Malleolar Screws
- 3.5 mm Malleolar Screws
- 4.5 mm Malleolar Screws
The most frequently used orthopedic implants are bone screws. For various types of bones, there are numerous types and sizes of screws. The majority of bone screws are constructed from titanium or stainless steel alloys. When determining screw mechanics, it’s important to consider the outer diameter, root diameter, thread pitch, and angle.
For example, a “7.5 mm Headless Compression Screw” has an outside diameter of 7.5 mm. In orthopedics, screws are typically described by their outer diameter. The linear distance covered by a screw during one complete turn is known as the pitch of the screw. With each full turn, the screw moves forward by a distance equal to the space between the threads. Cortical screws have more threads because they have a lower pitch. Given the fragility of the bone, cancellous bone screws have a deeper screw to increase surface area and enhance purchase.
Screws work by converting the torque applied to tighten them into internal tension and elastic responses in the bone around them. The fracture fragments that the screw is holding together are compressed as a result. Typically, screws are inserted into holes that have been drilled to the same diameter as the root and are either self-tapping or have been tapped (threaded) beforehand. The screws must be properly inserted into the proper size drilled hole and made to withstand the insertion torque levels anticipated in cortical bone because the torque to insert cortical bone screws can be high. Large, deep threads on cancellous bone screws allow them to securely hold the spongy bone. It is uncommon for a screw to fail during insertion due to the cancellous bone’s relatively low strength, but pull out can be problematic.
7.5 mm Headless Compression Screw Risk Factor
When assessing the prognosis in each case, contraindications—which may be partial or complete—must be taken into account. Under the following circumstances, alternative management strategies may need to be taken into account:
infections that are systemic or local, acute or chronic.
either localized, systemic, or chronic inflammation.
serve as a dangerous vascular, nervous, or muscular disease.
Bone defects that would prevent the implant from being properly anchored.
All associated illnesses that might jeopardize the implant’s success and functionality.
Warnings and Precautionary for 7.5 mm Headless Compression Screw
The surgeon and support staff should read the safety instructions in this document as well as any product-specific information in the product description, surgical techniques, and/or brochures before using the 7.5 mm Headless Compression Screw.
Screws are designed, built, and produced with the utmost care using materials of the highest quality for medical use. If these high-quality screws are used properly, they guarantee the best working outcomes. As a result, the usage guidelines and safety advice below must be followed.
The incorrect use of a screw can result in injury to the operator, patients, or other people as well as tissue damage, premature wear and tear, instrument destruction, and instrument destruction.
The operating surgeon must actively participate in the medical care of their patients. The surgeon must have a complete understanding of the instruments, their limitations, and the surgical procedure. The surgeon and the surgical team are responsible for exercising caution in the selection and use of surgical instruments. Before using implants, adequate surgical training should be obtained.
Factors that could harm the operation’s success include:
- allergies to materials implanted.
- regional bone tumors.
- osteomalacia or osteoporosis.
- metabolic disturbances and systemic disease.
- drug and alcohol abuse.
- Excessive shock-producing physical activity that exposes the implant to blows and/or heavy loads.
- Patients who lack the mental capacity to comprehend and follow instructions from a doctor.
- Unhealthy overall.
- Potential Negative Effects
The most frequent side effects following implantation are as follows:
- screw loosening that may be caused by the implant’s tissue reaction or by the fixation site’s repeated loading.
- the two stages of infection.
- additional bone fracture brought on by abnormal stress or weakened bone structure.
- a hematoma or pressure-related pressure that causes temporary or permanent neural damage.
- Hematomas from wounds and slow wound healing.
- Venous thrombosis, pulmonary embolism, and cardiac arrest are examples of vascular disease.
- heterotopically ossifying.
- suffering brought on by the 7.5 mm Headless Compression Screw.
- Implant mechanical failure, such as bending, loosening, or breakage.
- Implant migration leading to injury.
Preoperative Planning for 7.5 mm Headless Compression Screw
Following a thorough clinical evaluation of the patient, the operation is planned. X-rays are also necessary to provide a clear picture of the bony anatomy and any associated deformities. The necessary implantation tools as well as a full size 7.5 mm Headless Compression Screw must be on hand at the time of the procedure.
The potential risks and complications related to the use of implants should be discussed with the patient by the clinician. If the patient has allergies to any of the implant materials, it is crucial to know this before surgery. Additionally, the patient needs to be made aware that the device’s performance cannot be guaranteed because problems may reduce its lifespan.
7.5 mm Headless Compression Screw Precautions
During reprocessing, verify that the instruments are functional and look for wear. Before using, replace any worn-out or broken instruments.
It is advised to use the tools designated for this screw.
Use caution when handling equipment, and put used bone-cutting tools in a sharps container.
Always use suction and irrigation to remove any debris that may be produced during implantation or removal.
7.5 mm Headless Compression Screw Warnings
Headless Compression, 7.5 mm During use, a screw may break (if excessive forces are applied). We advise that the broken part be removed whenever possible and practical for the particular patient, though the surgeon will ultimately decide whether to do so based on the risk involved. Be aware that implants lack the natural bone’s strength. Significant loads may cause implants to fail.
The user’s glove or skin may be pinched or torn by the sharp edges or moving joints of some instruments, screws, and cut plates.
Be sure to get rid of any fragments that weren’t fixed during surgery.
While the surgeon will ultimately decide whether to remove the implant, we advise that fixation devices be taken out as soon as it is safe and practical for the specific patient and after their purpose as a healing aid has been fulfilled. To prevent refracture, implant removal should be followed by adequate post-operative care.
7.5 mm Headless Compression Screw General Adverse Events
There are risks, side effects, and adverse events associated with all major surgical procedures. While there are many possible reactions, the following are some of the most frequent ones: issues related to anesthesia and patient positioning (such as nausea, vomiting, dental injuries, neurological impairments, etc.), thrombosis, embolism, infection, damage to nerve and/or tooth roots or other critical structures, such as blood vessels, excessive bleeding, damage to soft tissues, including swelling, abnormal scar formation, functional impairment of the musculoskeletal system, and pain.
| 7.5 mm Headless Compression Screws, Full Thread |
|---|