Model No: 124433-A12
- Best Quality
- Affordable Pricing
- On-Time Delivery
- Customer Satisfaction
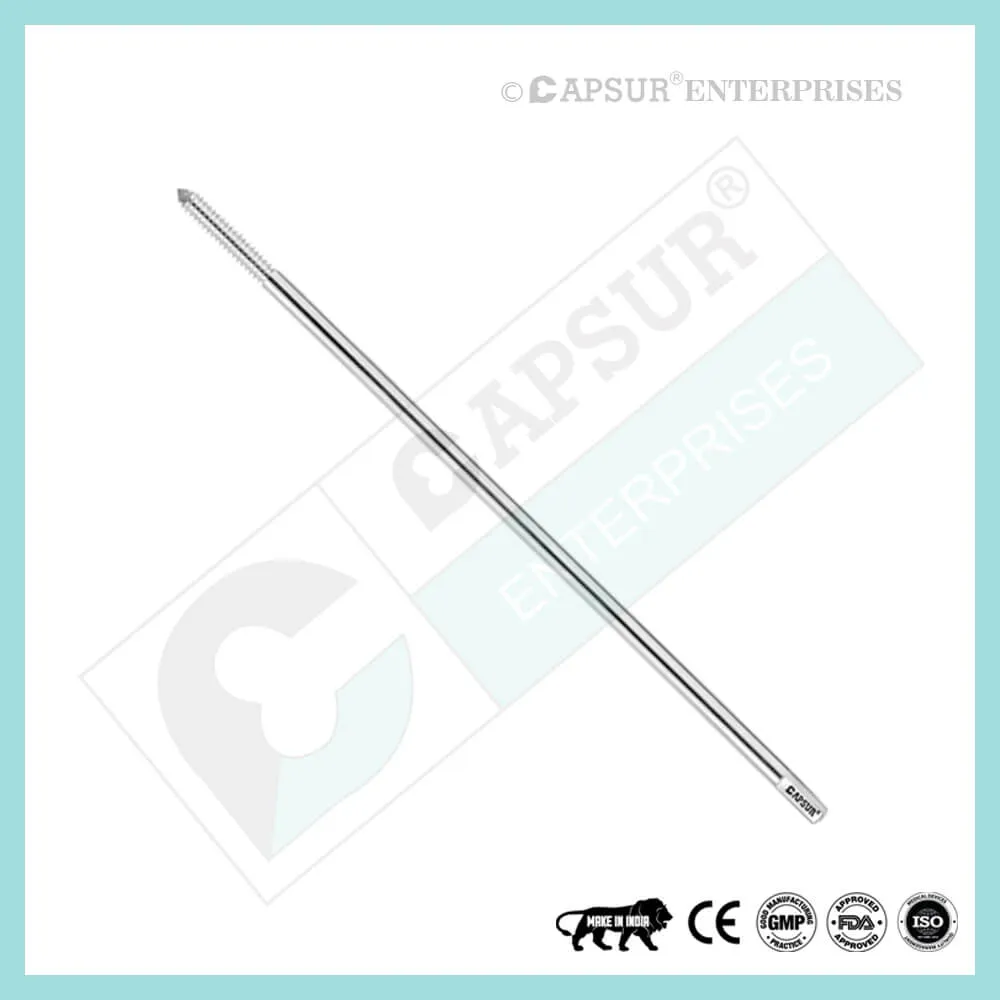
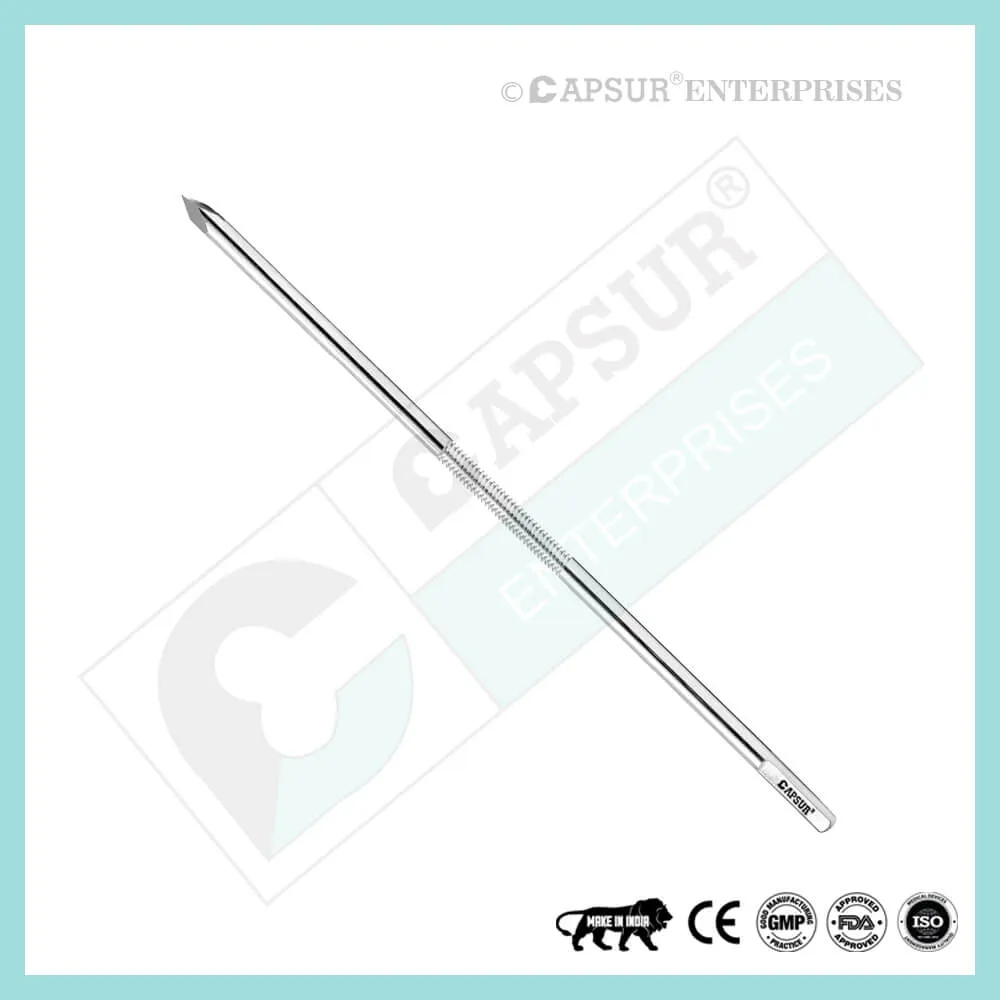
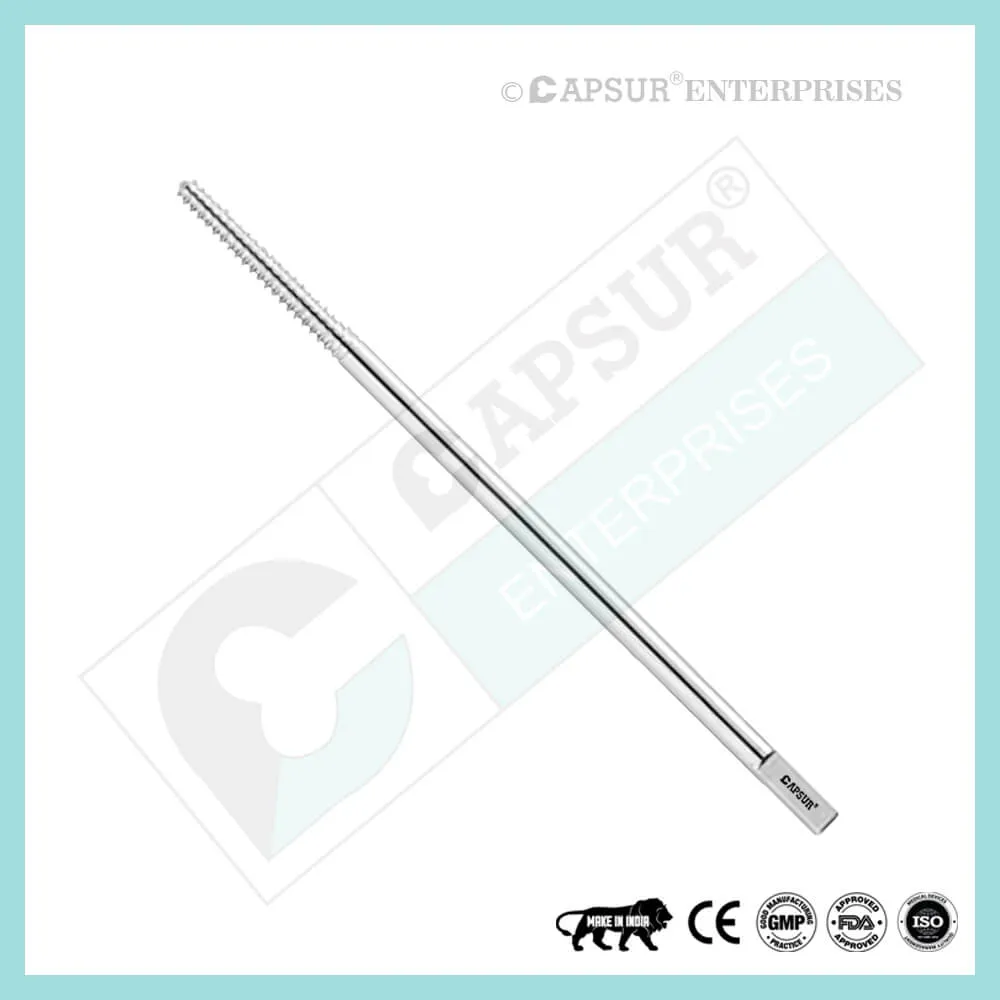
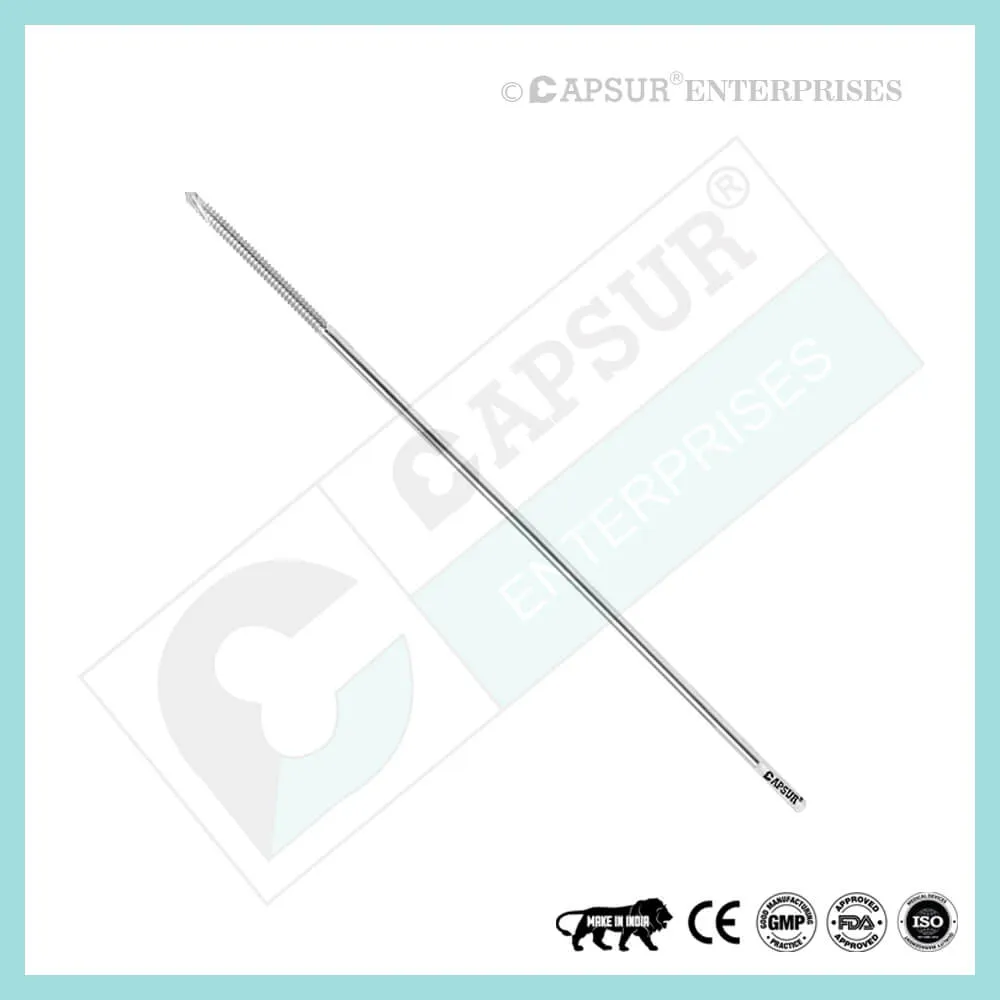
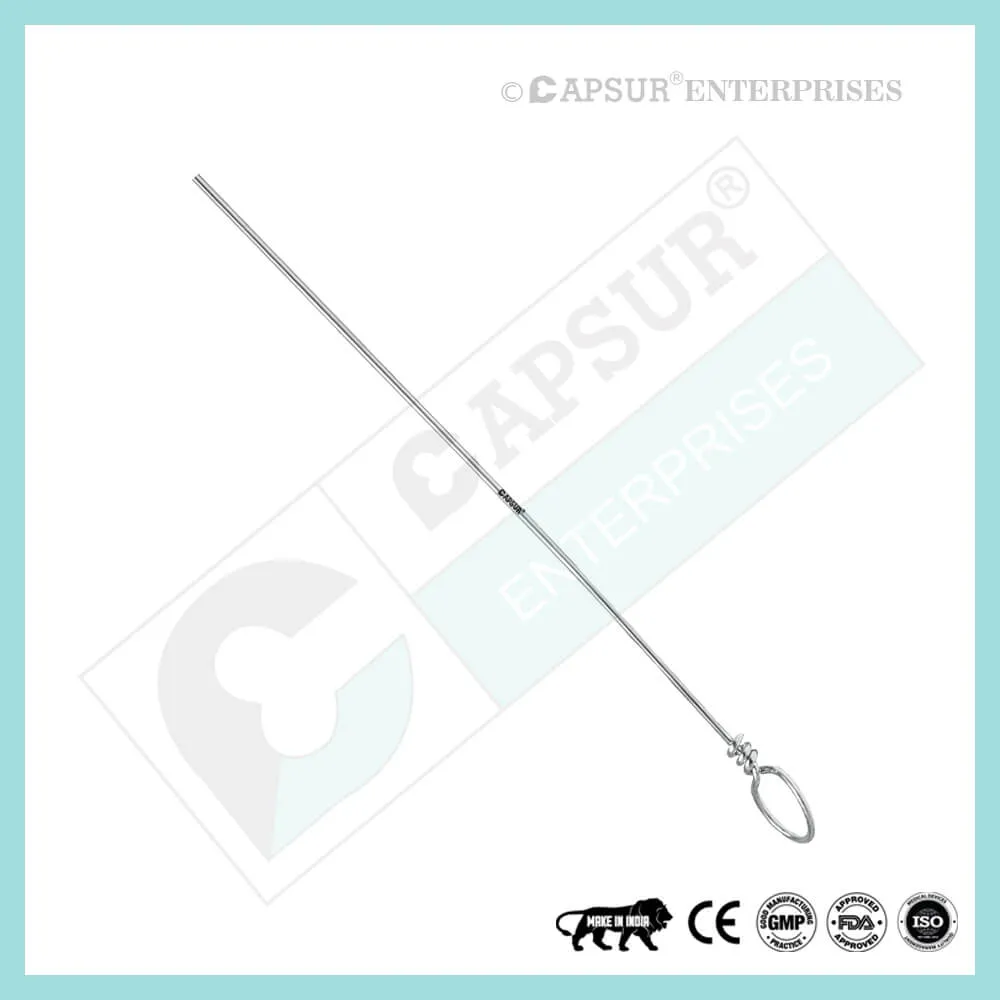
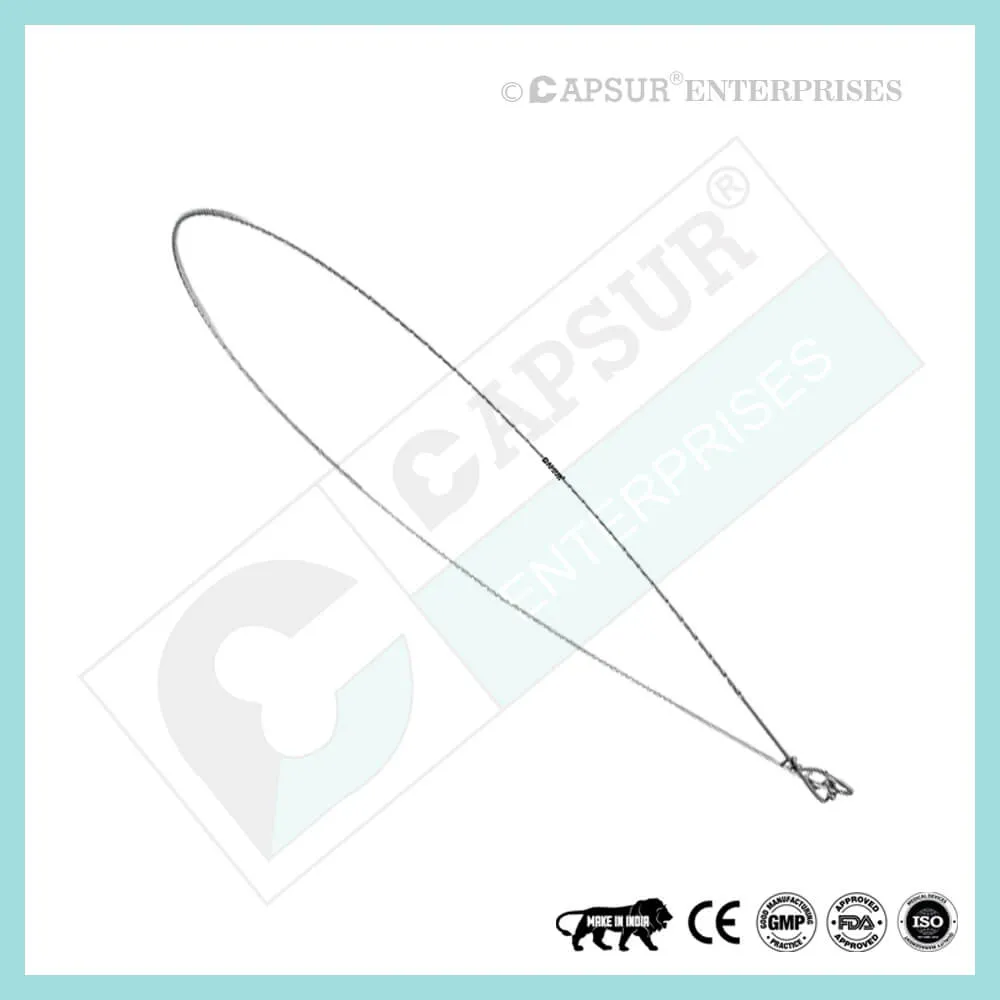
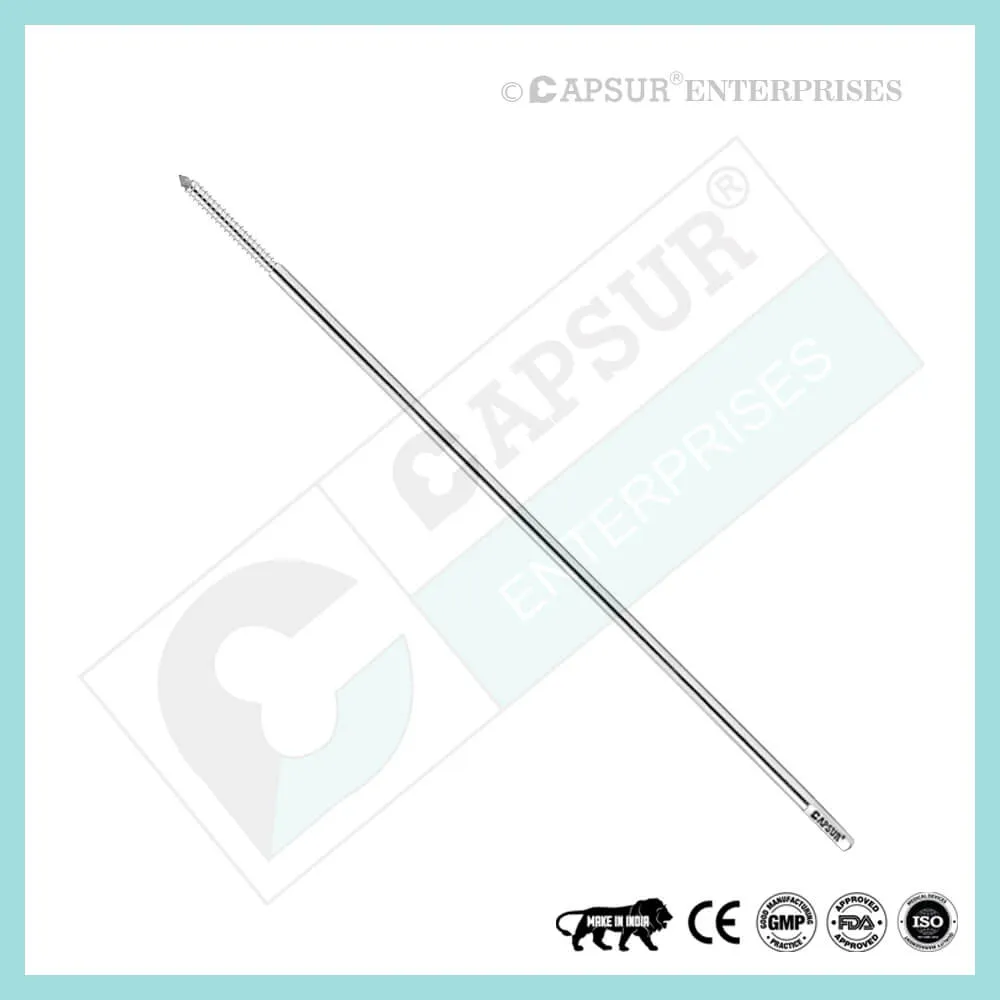
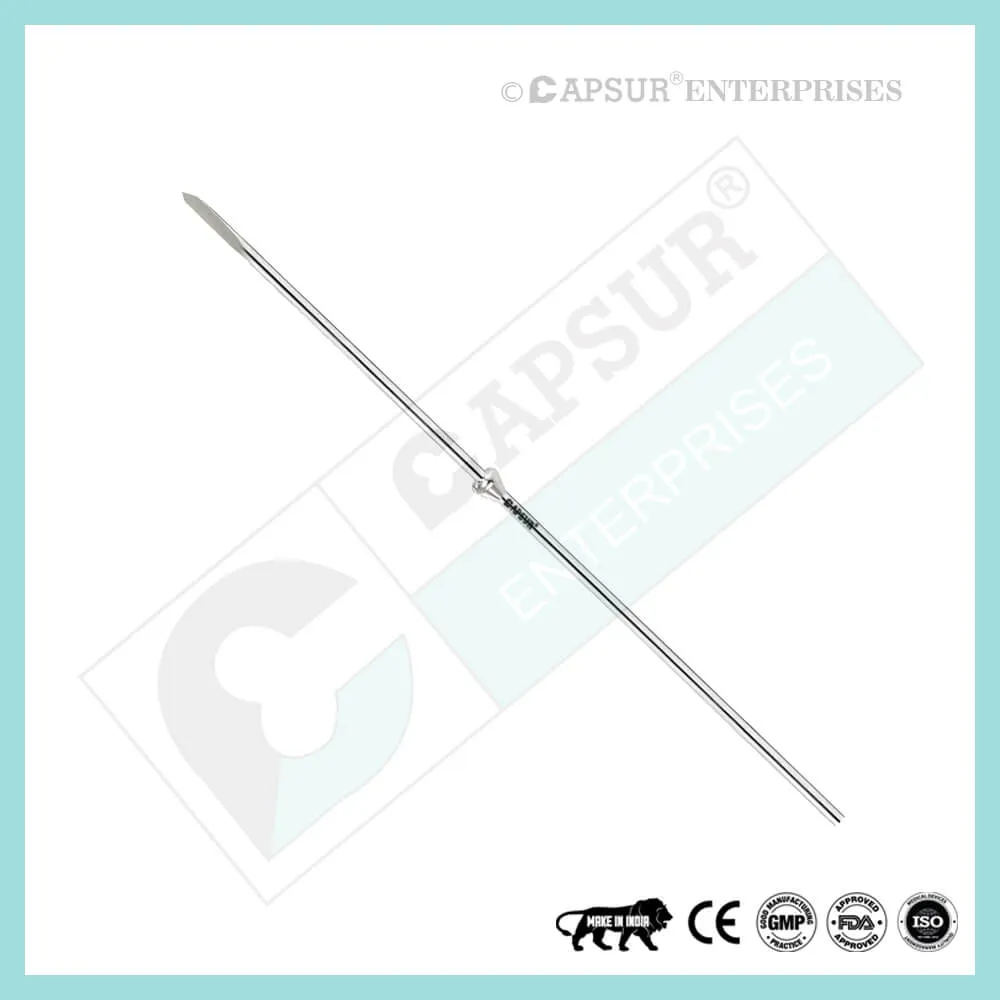
Specification of Guide Wire for PFN 2/2.5/3 x 400 mm
A guide wire is a small, flexible medical wire that is inserted into the body to direct a bigger tool. To ensure the highest quality, we use the best SS 316L material to make our guide wire PFN. The guide wire PFN has a 400 mm length and a diameter of 2 mm, 2.5 mm, or 3 mm.
Over a guide wire, most nails are inserted. Always work over a guide wire when reaming.
Under X-ray supervision, the Guide Wire PFN is inserted.
The fracture needs to be properly aligned in order to make it easier to pass the guide wire across the fracture site. The angulated tip may make it simpler to pass the guide wire.
If the fracture ends cannot be sufficiently aligned to allow a guide wire to pass, an aiming device may be inserted into the proximal fragment (following any necessary reaming) to manipulate the proximal fragment and allow the guide wire PFN to pass into the distal fragment.
By comparing a second guide wire of the same length to the one that has been inserted, it is possible to determine the nail’s exact length. Utilizing an image intensifier, it is important to check that the guide wire PFN is positioned properly in the distal canal. The second guide wire’s tip needs to be placed where it enters the bone.
Other Important Info of Guide Wire for PFN 2/2.5/3 x 400 mm
Guide Wire PFN Use in Intramedullary nailing
Insertion of a guide wire
Manual reamer
The guide wire PFN can typically be inserted into the diaphyseal medullary canal after the entry site has been prepared using one of the techniques. If there is still cancellous bone in the way, use a hand reamer to finish the entry. When the medullary canal is blocked by callus, these instruments (with diameters of 6, 7, and 8 mm) are also useful for treating old fractures and non-unions.
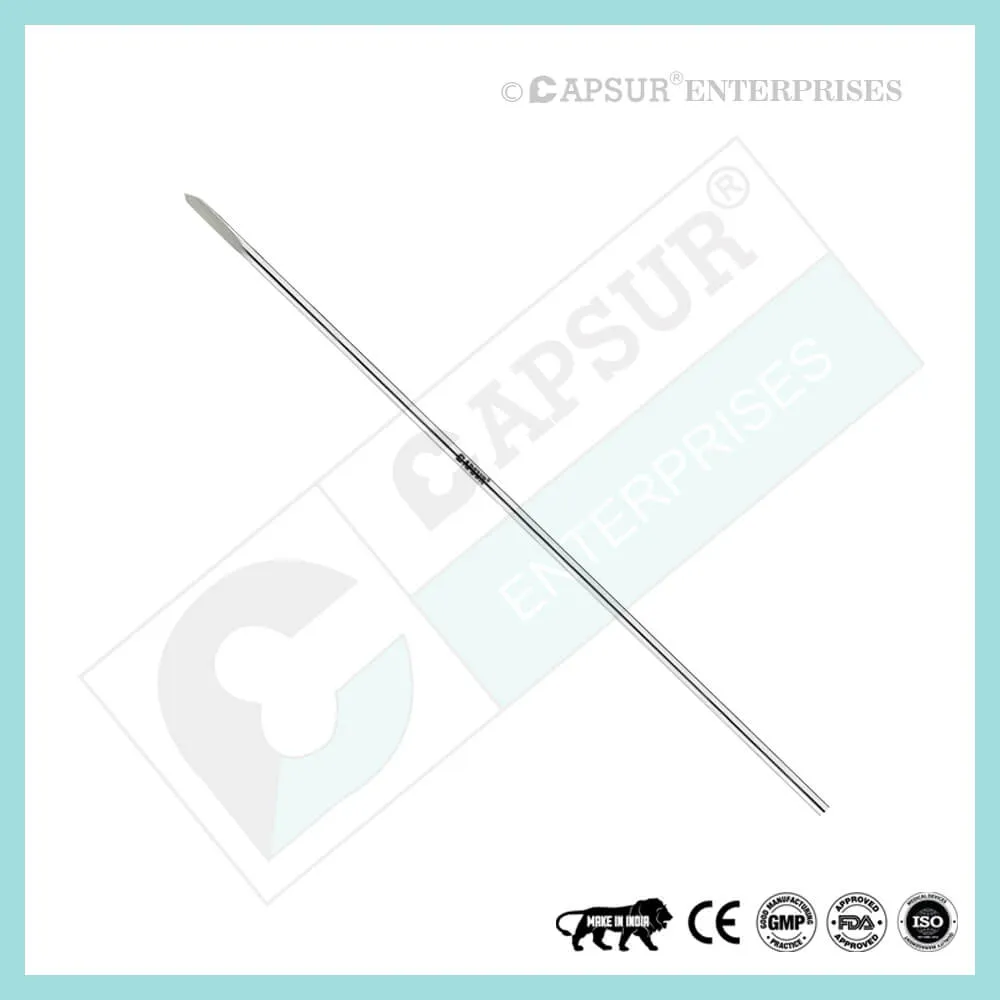
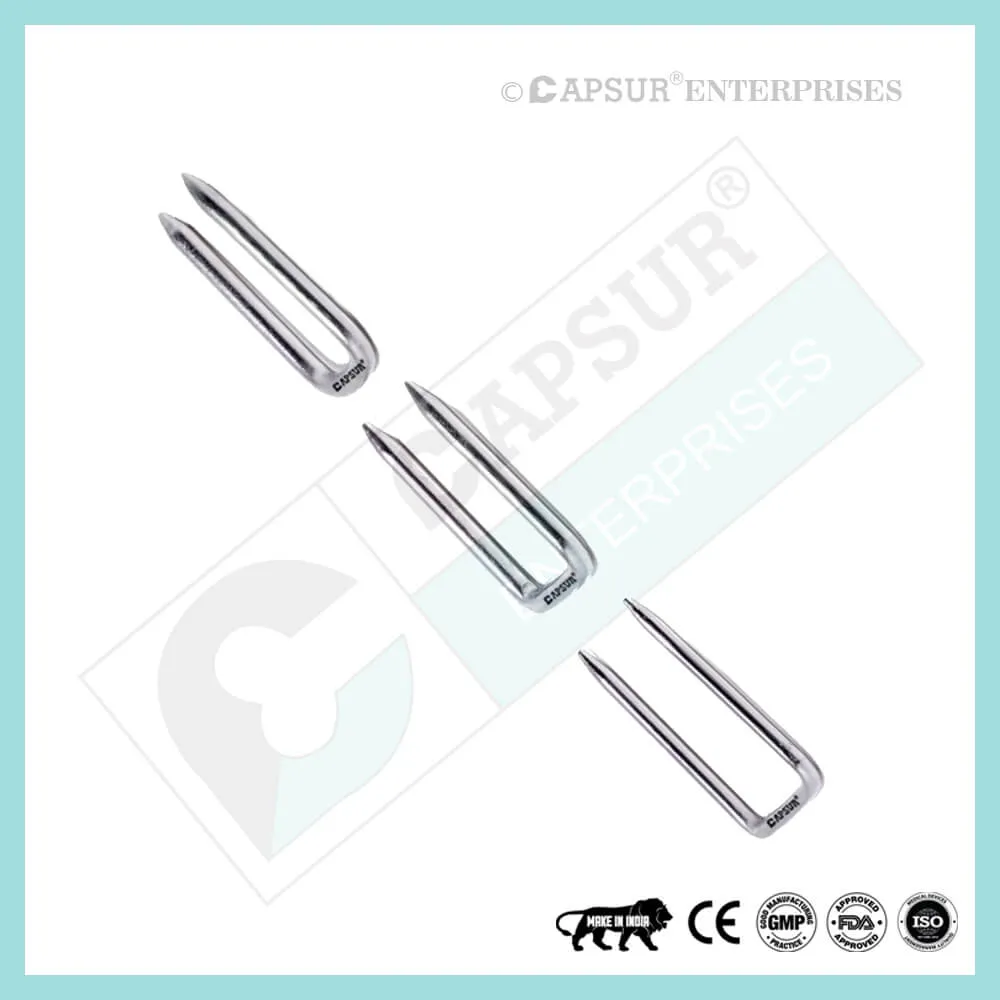
rounded-tip guide wire
Pass a ball tip guide wire into the distal metaphysis through the medullary canal after the proximal metaphysis has been broken. Reduction of the fracture is necessary. Special efforts might be needed if fracture reduction is challenging or the fracture has become comminuted.
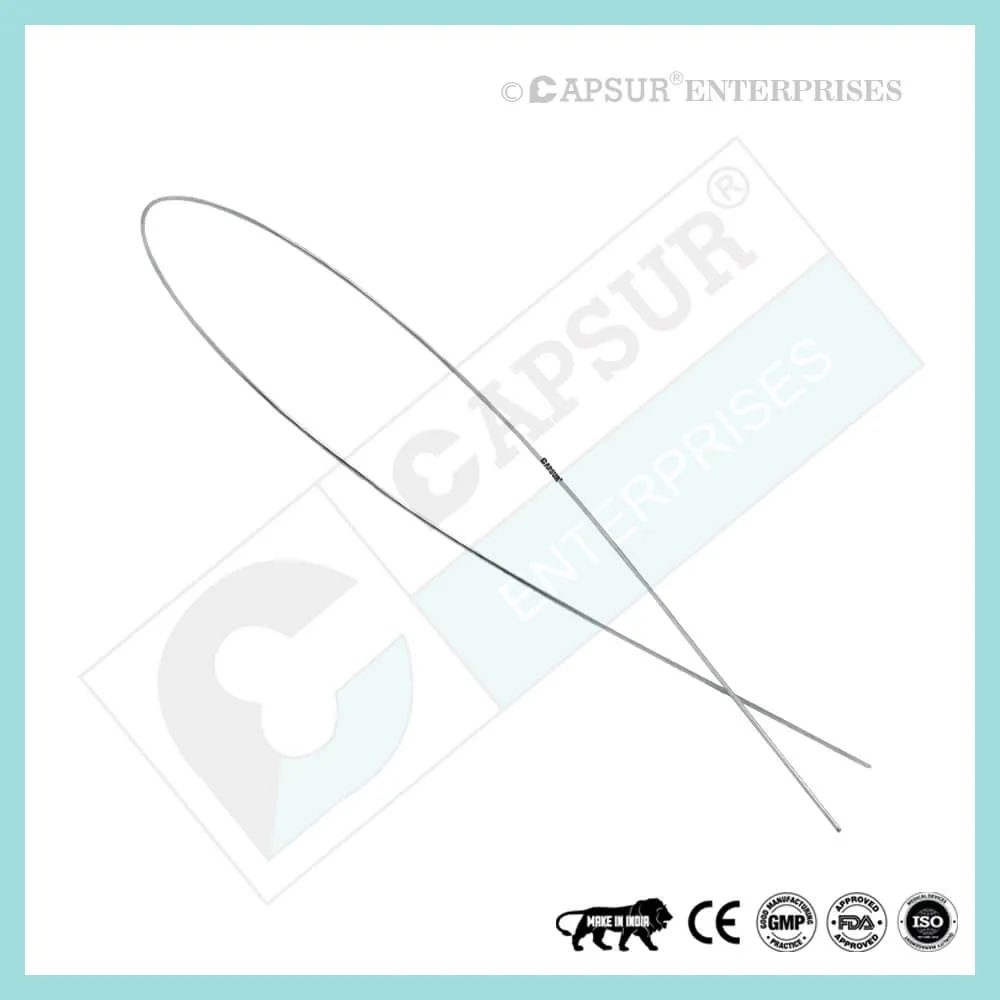
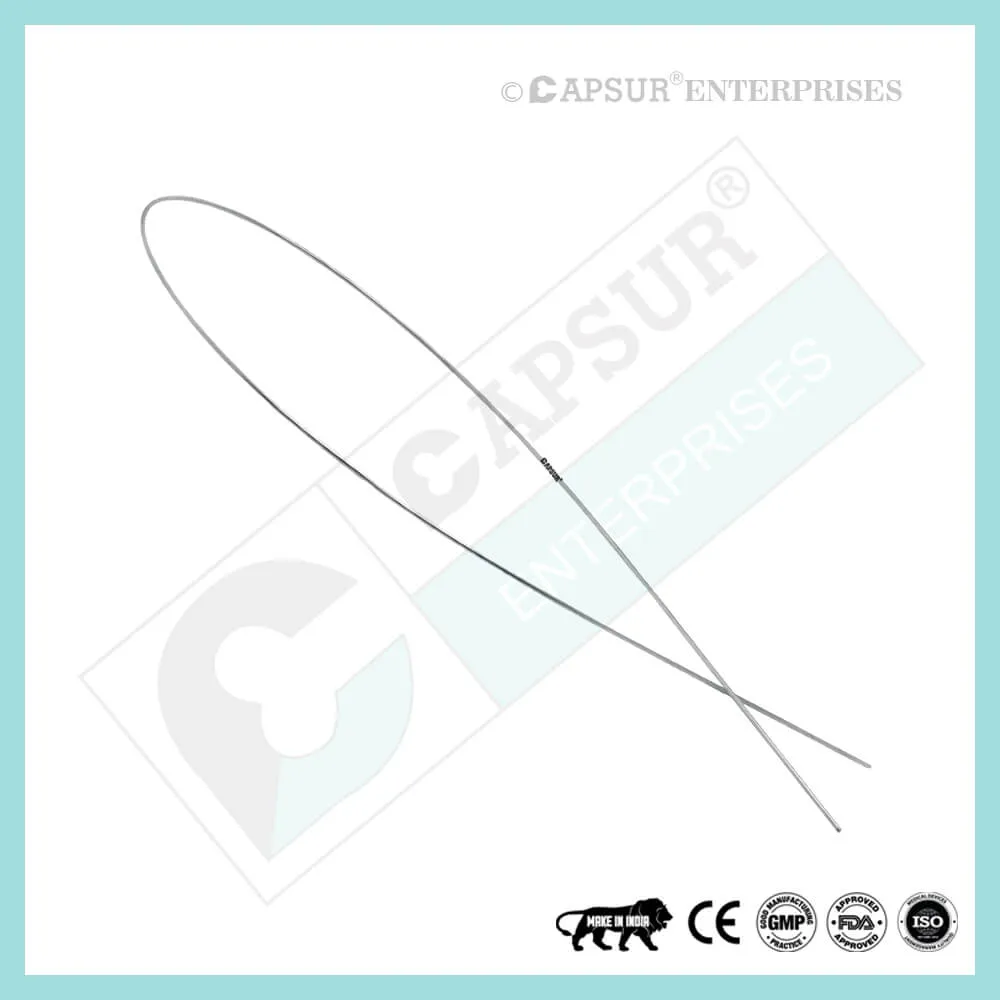
the guide wire being bent
Two benefits result from slightly bending the guide wire 10-15 mm above its tip:
- Because the wire’s tip is redirected by rotation, it is simpler to pass through the fracture site and into the distal fragment.
- It also makes it easier for the tip to be placed correctly in the distal metaphysis.
The bend can be placed beyond the ball of a guide wire PFN with its ball slightly proximal to the end, preventing jamming inside a cannulated reamer.
control using fluorescence
Check that the guide wire is above the middle of the ankle joint using fluoroscopy.
determining the length of a nail
Nail size
Preoperative nail length estimation is done, but intraoperative measurement is more accurate. Utilize the radiographic ruler that was included with the nail’s tools. Measure the distance from the intended nail entry site to just above the ankle joint after the fracture has healed.
Choose a nail that penetrates only the surface of the bone from the distal tibia to the entry point. When treating distal fractures, nail length might be crucial. To compensate for an excessively short nail, some nails have proximal extensions of various lengths that can be added after insertion.
A straightforward, clinical intraoperative length measurement is suggested if a radiographic ruler and/or image intensifier are not available. Place a second guide wire of equal length at the entry portal while the intramedullary guide wire PFN is in the correct position. Then, measure the length difference between the two wires.
reaming and measuring the diameter of the nails
Reaming
Over the ball-tipped guide wire, place the flexible-shaft reamer with a cannula.
Starting with an end-cutting reamer, increase the reamer diameter incrementally, typically by 0.5 mm. During this process, use a reamer sleeve, as shown, or suitable retractors to protect the soft tissues at the entry site.
Reamer should not be pushed! Pull back a little every so often as you advance to clear the medullary canal of debris.
The reamer is in contact with the internal cortical surface when there is a chattering sensation. An appropriate diameter nail can usually be passed with an additional millimeter or two of reaming.
selecting the nail diameter
A radiographic gauge is used to measure the diameter of the medullary canal. Check the lateral and AP views.
The nail diameter must be sufficient to ensure the strength and longevity of both the nail and the locking screws. Seek advice from the manufacturer of the nails. A 10 mm nail is typically adequate. Given that the medullary canal is not perfectly straight, reaming should be done to a diameter of 0.5 to 1.5 mm greater than the nail.
Getting ready to insert a nail
Nails with cannulas are inserted over the proper guide wires. For a solid nail, no wire is used. It might be impossible to remove the ball-tipped or severely bent guide wire tibia through a particular cannulated nail. If so, a new wire needs to be installed before the nail is put in. For changing guide wires, a plastic medullary exchange tube is available. Pass the medullary tube completely past the fracture site and over the reaming guide wire. While removing the reaming guide wire, keep it steady.
Check the distal tibia’s position in the tube after inserting the nailing wire there (AP and lateral x-rays). The medullary exchange tube should then be removed.
Putting the cannulated nail in
Inserting nails
The cannulated nail should be able to be inserted over the guide wire PFN by hand or with light hammering with enough reduction and over-reaming. Make sure to keep the fracture reduced as the nail crosses it. If insertion is challenging, ream to a larger diameter and/or correct the reduction.
To lessen the chance of knee pain, make sure the proximal end of the nail is buried beneath the surface of the bone at the entry site. For distal fractures in particular, careful nail length selection may be required to guarantee distal fixation and the correct length proximally.
The distal tibia’s middle should be where the nail tip is positioned, roughly at the level of the physeal scar (a denser bone). For fractures below the medullary isthmus, it is crucial to place the nail distally. The surgeon must maintain proper fracture alignment because, at this level, nail passage does not weaken the fracture.
Pitfalls
Each time you tap the hammer on the nail, the nail should move closer to the medullary canal. If resistance is felt, it might be because the entry point was chosen incorrectly or because the distal fragment’s cortex was struck by the nail tip.
Forced hammering can result in nail incarceration, fracture comminution, or nail twisting.
Guide Wire PFN Risk Factor
When assessing the prognosis in each case, contraindications—which may be partial or complete—must be taken into account. Under the following circumstances, alternative management strategies may need to be taken into account:
- infections that are systemic or local, acute or chronic.
- either localized, systemic, or chronic inflammation.
- serve as a dangerous vascular, nervous, or muscular disease.
- Bone defects that would prevent the implant from being properly anchored.
- All associated illnesses that might jeopardize the implant’s success and functionality.
Warnings and Precautionary for Guide Wire PFN
The surgeon and support personnel should read the safety instructions in this document as well as any product-specific information in the product description, surgical techniques, and/or brochures before using Guide Wire PFN.
Guide Wire PFN is made with medical-grade materials and is carefully designed, built, and produced. If used properly, these high-quality guide wire PFN ensure the best working outcomes. As a result, the usage guidelines and safety advice below must be followed.
Inappropriate use of guide wires can result in injury to the operator, patients, or other people as well as tissue damage, premature wear and tear, instrument destruction, and instrument destruction.
The operating surgeon must actively participate in the medical care of their patients. The surgeon must have a complete understanding of the instruments, their limitations, and the surgical procedure. The surgeon and the surgical team are responsible for exercising caution in the selection and use of surgical instruments. Before using implants, adequate surgical training should be obtained.
Factors that could harm the operation’s success include:
- allergies to materials implanted.
- regional bone tumors.
- osteomalacia or osteoporosis.
- metabolic disturbances and systemic disease.
- drug and alcohol abuse.
- Excessive shock-producing physical activity that exposes the implant to blows and/or heavy loads.
- Patients who lack the mental capacity to comprehend and follow instructions from a doctor.
- Unhealthy overall.
- Potential Negative Effects
- The most frequent side effects following implantation are as follows:
- cyclic loading of the fixation site and/or tissue reaction to the implant may cause the guide wire to loosen.
- the two stages of infection.
- additional bone fracture brought on by abnormal stress or weakened bone structure.
- a hematoma or pressure-related pressure that causes temporary or permanent neural damage.
- Hematomas from wounds and slow wound healing.
- Venous thrombosis, pulmonary embolism, and cardiac arrest are examples of vascular disease.
- heterotopically ossifying.
- Due to the Guide Wire PFN’s presence, there is pain and discomfort.
- Implant mechanical failure, such as bending, loosening, or breakage.
- Implant migration leading to injury.
Preoperative Planning for Guide Wire PFN
Following a thorough clinical evaluation of the patient, the operation is planned. X-rays are also necessary to provide a clear picture of the bony anatomy and any associated deformities. Along with a full size of Guide Wire PFN, the appropriate implantation tools must be on hand when the procedure is performed.
The potential risks and complications related to the use of implants should be discussed with the patient by the clinician. If the patient has allergies to any of the implant materials, it is crucial to know this before surgery. Additionally, the patient needs to be made aware that the device’s performance cannot be guaranteed because problems may reduce its lifespan.
Guide Wire PFN Precautions
During reprocessing, verify that the instruments are functional and look for wear. Before using, replace any worn-out or broken instruments.
Utilizing the tools listed for this Guide Wire PFN is advised.
Use caution when handling equipment, and put used bone-cutting tools in a sharps container.
Always use suction and irrigation to remove any debris that may be produced during implantation or removal.
Guide Wire PFN Warnings
When put through excessive force, Guide Wire PFN can break while in use. We advise that, whenever possible and practical for the particular patient, the broken part should be removed. The surgeon will ultimately decide whether to remove the broken part based on the risk involved. Be aware that implants lack native bone’s tensile strength. Implants that are subjected to heavy loads may fail.
Sharp edges or moving joints on tools, screws, and cut plates could rip or pinch the user’s glove or skin.
Make sure to get rid of any fragments that weren’t surgically fixed.
The final decision to remove an implant rests with the surgeon, but we advise that fixation devices be taken out as soon as it is safe and practical for the particular patient and after their purpose as a healing aid has been fulfilled. To prevent refracture, adequate post-operative management should be performed after removing the guide wire.
Guide Wire PFN General Adverse Events
There are risks, side effects, and adverse events associated with all major surgical procedures. While there are many possible reactions, the following are some of the most frequent ones: issues related to anesthesia and patient positioning (such as nausea, vomiting, dental injuries, neurological impairments, etc.), thrombosis, embolism, infection, damage to nerve and/or tooth roots or other critical structures, such as blood vessels, excessive bleeding, damage to soft tissues, including swelling, abnormal scar formation, functional impairment of the musculoskeletal system, and pain.
| Guide Wire for PFN 2/2.5/3 x 400 mm |
|---|